Abstract
Objective
The aim of the study was to evaluate the ability of home ventilators to maintain a minimal tidal volume during different conditions associated with alveolar hypoventilation.
Design
Bench evaluation coupled with an in vivo study on two healthy subjects.
Setting
Tertiary university hospital and research unit.
Interventions
Six ventilators having a “volume guarantee” module (Synchrony II, Philips Respironics; Vivo 40, Breas; Legendair, Airox; Elisee 150, Philips Respironics; Ventimotion, Weinmann; and VS III, Resmed) were tested on a lung bench in a baseline condition and in three conditions associated with alveolar hypoventilation: increase in airway resistance, decrease in lung compliance, and non-intentional leaks. An in vivo study completed the bench study for the non-intentional leak condition.
Measurements and results
The six ventilators were able to maintain a minimal tidal volume during an increase in airway resistance and a decrease in lung compliance. The maintenance of a minimal tidal volume during a non-intentional leak was more difficult and was associated with large variations in tidal volume, a default of pressure support delivery for some devices, and patient-ventilator dyssynchrony, both during the bench and the in vivo study.
Conclusions
The six home ventilators tested in the study were able to maintain a minimal tidal volume during an increase in airway resistance and a decrease in lung compliance, but not during a non-intentional leak.
Similar content being viewed by others
Introduction
The aim of non-invasive positive pressure ventilation (NPPV) is to maintain a minimum level of alveolar ventilation during prolonged periods, usually the night. But, even in a resting condition such as sleep, breathing pattern is not stable. Regular changes in respiratory mechanics may occur, due to variations in central drive, lung mechanics, and respiratory and upper airway muscle tone and activity. Changes in respiratory impedance may be observed during changes in body position [1]. During sleep, the physiological decrease in upper airway muscle activity increases airway resistance. These changes, which are exaggerated in pathologic conditions, may decrease tidal volume (V t) and promote hypercapnia. Leaks are unavoidable during NPPV and a major cause of persistent nocturnal hypercapnia [2, 3].
Home ventilators tend to integrate continuously new options and measures. A module that guarantees a minimal V t is available on some home ventilators. The principle of this “volume guarantee” module is based on the automatic detection of the expired V t by the ventilator. When the expired V t falls below a fixed threshold, the ventilator increases the inspiratory positive airway pressure (IPAP) and eventually the inspiratory time (T i) until the delivered V t reaches a minimum V t. Also, after the resolution of a pathological condition, the ventilator should be able to return to its baseline settings while preserving the patient ventilator synchrony. The aim of this “volume guarantee” module is thus to combine a minimum level of alveolar ventilation with the maximal patient comfort. However, we have observed in our clinical experience that the ability of a ventilator to respond to different conditions, i.e., changes in compliance or resistance or air leaks, varies among different devices.
The aim of our study was to verify the ability of home ventilators having a “volume guarantee” module to effectively deliver a minimal V t during three common clinical situations: increase in airway resistance, decrease in lung compliance, and a non-intentional leak. An in vivo study on healthy subjects completed the bench study.
Materials and methods
Experimental in vitro study
All home ventilators having a “volume guarantee” were tested (Table 1).
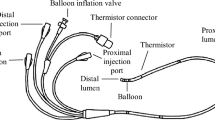
The bench used for this study has been described and consisted in a two-chamber Michigan test lung (MII Vent Aid TTL; Michigan Instrument, Grand Rapids, MI) [4, 5]. Each tested ventilator was connected via its standard circuit (simple and/or double when available) to the first chamber of the test lung, the second chamber (driving chamber) being connected to a flow-rate generator that could produce various wave forms. The two chambers were physically connected by a small metal component that allowed the driving chamber to lift the testing chamber. The resistance was a parabolic airway resistor (Pneuflo® Airway resistor Rp5, Rp20, Rp50 or Rp200; Michigan Instrument, Grand Rapids, MI). A leak valve was added to simulate a non-intentional leak.
Pressure (Paw) and flow were measured at the end of the ventilator circuit using a pressure differential transducer (Validyne DP 45 ± 56 cmH2O, Northridge, CA) and a pneumotachograph (Fleisch n°2, Lausanne, Switzerland) associated with a pressure differential transducer (Validyne DP 45 ± 3.5 cmH2O). The leak flow was measured with a second pneumotachograph. Signals were digitised at 200 Hz by an analogic/digital system (MP100, Biopac Systems, Goleta, CA) and recorded on a microcomputer.
Determination of the baseline profile for each ventilator
A patient profile having respiratory mechanics with a parabolic airway resistor [Pneuflo® Airway resistor Rp5: ΔP 2.7 × V with ΔP pressure drop (cmH2O) V flow rate (l/s) and a compliance of 100 ml/cmH2O] was simulated on the bench. The spontaneous breathing pattern associated a V t of 300 ml, a breathing rate of 12 breaths/min and a T i of 1 s.
Each ventilator was connected to the bench, the “volume guarantee” module being inactivated. For each ventilator, positive end-expiratory pressure (PEEP) was set at 4 cmH2O, inspiratory trigger was set at its most sensitive value that did not induce auto-triggering, and expiration was authorized when the inspiratory flow fell below 25% of peak inspiratory flow. The IPAP was then set at a value that allowed a V t of 600 ml. Above this IPAP value, the range of IPAP variations was set between ±8 cmH2O. This setting was the baseline condition.
Determination of the perturbations altering the V t for each ventilator
After the determination of the baseline profile, the values of airway resistance (condition R), lung compliance (condition C), and leaks (condition L) that resulted in a decrease of V t from 600 to 400 ml (−33%, i.e., a threshold associated with persistent hypercapnia in chronic respiratory failure patients treated at home by mechanical ventilation [2, 3]) were determined for each ventilator.
The experimental protocol
Sixty respiratory cycles were recorded as the baseline condition for each ventilator after having set the “volume guarantee” module at 550 ml (baseline condition). Then, the R, C, and L conditions were tested in a random order during 60 respiratory cycles. Finally, 60 respiratory cycles were recorded after the correction of the pathological condition (return to baseline condition). “Volume guarantee failure” was defined arbitrarily as the inability to maintain a V t of at least 500 ml during a pathological condition. An “overshoot” was defined as a V t > 650 ml. Patient-ventilator dyssynchrony comprised (1) auto-triggering, defined by the delivery of a cycle by the ventilator without a prior breath initiated by the driving chamber, (2) lack of detection of the patient’s inspiratory effort, defined by the lack of delivery of a cycle by the ventilator despite the initiation of a breath by the driving chamber, and (3) failure of pressure support, defined by the inability of the ventilator to reach the required IPAP.
In vivo study
In order to check the clinical relevance of the results obtained with the bench study, an in vivo study on two healthy subjects was designed. This study aimed to test the most critical situation (i.e., leaks) by using in a clinical setup the three ventilators exhibiting during the bench test study different and representative patterns of response; a ventilator that was able to cope with leaks (Synchrony II), a ventilator that imperfectly coped with leaks with the occurrence of delayed patient-ventilator dyssynchrony (Vivo 40), and a ventilator that was unable to cope with leaks with immediate patient-ventilator dyssynchrony (Ventimotion). The subjects breathed 2 min without leaks, followed by 2 min with inspiratory mouth leaks to simulate a non-intentional leak [6], and finally 2 min after mouth closure. This clinical study was approved by the local ethics committee, and written informed consents were obtained from the two subjects.
Analysis of the data
The following parameters were computed from each pressure and/or flow trace: IPAP, PEEP, V t, and T i. Because the number of subjects tested in the in vivo study was too small, the comparison was only qualitative.
Results
Increase in airway resistance
All the ventilators, except the Ventimotion (maximal V t = 445 ml), were able to guarantee a minimal V t of 500 ml (Fig. 1 and see online supplement Tables 1–9). The time response of the ventilator varied from 1 (Vivo 40, Legendair simple circuit, Elisee 150 double circuit, VS III simple and double circuit) to 14 breathing cycles (Synchrony II). A minimal V t could be reached because of a 3 (Ventimotion) to 10 cmH2O (Synchrony II and Legendair double circuit) increase in IPAP. However, an overshoot was observed with the Synchrony II (V t = 900 ml). This increase of IPAP was associated with an increase of the T i in three ventilators (Synchrony II, Vivo 40, Legendair simple and double circuit). After the return to the baseline resistance, V t increased with all the six devices, from 770 ml (Elisee double circuit) to 1,360 ml (Legendair double circuit). The return to baseline V t values was observed after 1 (VS III simple and double circuit) to 51 (Ventimotion) breathing cycles. A typical tracing is shown in Fig. 2.
Evolution of the tidal volume (V t) and the inspiratory airway pressure (IPAP) during the three conditions: increase in airway resistance, decrease in lung compliance, and the presence of a non-intentional leak for the six ventilators. *Autotriggering and patient ventilator dyssynchrony, $autotriggering and patient ventilator dyssynchrony and failure of pressure support, £autotriggering (breathing frequency increases twofold)
Decrease in lung compliance
All the ventilators, except the Vivo 40 (maximal V t = 490 ml), were able to guarantee a minimal V t of 500 ml (Fig. 1 and see online supplement Tables 1–9). The time response of the ventilator varied from 1 (Legendair double circuit, Elisee 150 simple and double circuit, VS III simple and double circuit) to 13 breathing cycles (Synchrony II). A minimal V t could be reached because of a moderate (1.6–3.3 cmH2O) increase in IPAP for all the ventilators. No overshoot was observed. After the return to the baseline compliance, V t increased with all the six devices, from 814 ml (VS III double circuit) to 1,045 ml (VS III simple circuit). The return to baseline V t values was observed after 1 (VS III simple and double circuit) to 27 (Ventimotion) breathing cycles.
Non-intentional leak
Only one ventilator (Synchrony II) was able to guarantee a minimal V t of 500 ml without patient ventilator dyssynchrony but an overshoot was observed (725 ml, Fig. 1 and see online supplement Tables 1–9). Patient ventilator dyssynchrony (essentially auto-triggering) was observed with all the other devices. With the Synchrony II, IPAP increased to 16.5 cmH2O. The time response of the ventilator was three breathing cycles. This increase of IPAP was associated with an increase in T i. After the resolution of the non-intentional leak, V t increased to 1,030 ml. The return to baseline V t values was observed after 22 breathing cycles. The Elisee 150 was not able to return to the baseline condition after the resolution of the non-intentional leak with patient ventilator dyssynchrony persisting during 17–30 breathing cycles.
In vivo study
During a non-intentional leak, the Synchrony II was not able to maintain the baseline V t, and IPAP did not increase (Table 2; Fig. 3). Autotriggering occurred during 19–38% of the breathing cycles. After the resolution of the non-intentional leak, IPAP returned to the baseline value, but V t overreached the baseline value by 50–300 ml.
The Vivo 40 was able to maintain the baseline V t because of a 2.5–3.3 cmH2O increase in IPAP. Autotriggering occurred during 12–16% of the breathing cycles. After the resolution of the non-intentional leak, IPAP was moderately lower (−2.3 cmH2O) or higher (+2.4 cmH2O) than the baseline IPAP with a 230 ml lower V t in one subject.
During NPPV with the Ventimotion, V t could not be maintained in one subject and increased, without reaching the baseline values, after the resolution of the non-intentional leak. IPAP remained within the baseline value during and after the resolution of the non-intentional leak.
Discussion
This study gives important messages with regard to the “volume guarantee” module of six home ventilators: (1) the coping with a non-intentional leak is more difficult than the coping with an increase in airway resistance or a decrease in lung compliance; (2) ventilators maintain a minimal V t by increasing IPAP, and, to a lesser extent T i; (3) an overshoot for V t is commonly observed, especially after the resolution of the pathological condition; (4) a non-intentional leak is associated with patient ventilator dyssynchrony in most ventilators; (5) the performance of the ventilators, with regard to their ability to respond to a pathological situation and its resolution, varied widely, no ventilator being able to adequately deliver a minimal V t without an overshoot and/or patient-ventilator dyssynchrony in the three conditions.
The occurrence of non-intentional leaks is a common cause of NPPV failure, patient ventilator dyssynchrony, and poor sleep quality. Leaks can be minimised by using a chin strap or a face mask, but they remain a major cause of ineffective ventilation and persistent hypercapnia [2, 7]. This risk of non-intentional leaks is one rationale for a “volume guarantee” module. A volume targeting ventilation has been evaluated in obesity-hypoventilation syndrome with conflicting results [8, 9]. Nocturnal transcutaneous pCO2 decreased significantly when using a volume guarantee module compared to a classical mode [8]. The variance of peak IPAP increased but without significant impact on sleep quality [8]. On the opposite, in another study, mean V t and minute ventilation increased with volume targeting, but at the expense of a reduced sleep time and more awakenings [9]. Such discrepancies can be explained by different V t settings leading to higher IPAP during sleep [10]. Accordingly, in patients with obstructive sleep apnea, it has been demonstrated, when using auto-titrating devices, that sleep structure correlates with pressure variations [11]. Our study showed that to maintain V t, some devices needed peak IPAP variations up to 10 cmH2O. Further studies are required to evaluate consequences of such pressure swings in terms of sleep fragmentation.
Breathing pattern is not stable, even during sleep. A pathological condition associated with alveolar hypoventilation may thus resolve spontaneously, after a variable time period. Ideally, a ventilator should be able to respond rapidly to changes in the effective V t after, respectively, the occurrence and resolution of leaks or changes in respiratory system impedance. In this study, this was observed with the Vivo 40, the Elisee, the Legendair, and the VS III. When leaks occur during sleep, this phenomenon may be relatively transient. However, leaks may cause sleep fragmentation and blood gases alteration [12, 13]. Therefore, in order to combine an efficient “volume guarantee” with the preservation of patient ventilator synchrony and sleep quality, the time response of the ventilator should be appropriate and probably smoother than the delay between the occurrence and the resolution of leaks [12, 13]. Indeed, an overshoot of V t, as observed in the present study with some devices, may cause hyperventilation and a decrease in the patient’s respiratory effort, causing patient-ventilator dyssynchrony [14] and possibly air leak injury. Moreover, these overshoots with high pressure levels may lead to a low pCO2 crossing the apnea threshold, favoring the occurrence or periodic breathing, oxygen desaturations, and microaraousals [15, 16]. Therefore, we believe that an ideal “volume guarantee” system should be targeted for transient and variable changes in leak severity or respiratory system impedance. As such, by using a prototype that adjusted the T i in less than three cycles and thereafter the IPAP in less than five cycles, no alteration of sleep parameters was observed in neuromuscular patients [17]. Similarly, the VS III, which responded very quickly in our study, was associated with a comparable control of nocturnal oxygenation as a standard NPPV, without altering sleep quality in stable neuromuscular and chest wall disease patients [18]. In contrast, Janssens et al. [9], who used the precursor of the Synchrony II, which needed at least 13 cycles to reach the volume guarantee in our study, observed in obesity-hypoventilation syndrome that this volume guarantee system altered sleep parameters. The apparent discrepancy between these studies can be attributed to differences in patient populations rather than to differences in devices and modules [19]. Therefore, more sleep studies in different patient populations are needed to confirm or reject the hypothesis that a delayed response of some “volume guarantee” systems could be harmful during sleep.
Persistent patient ventilator dyssynchrony, even after the resolution of a pathological event, may cause poor NPPV tolerance. An association has been observed between the reduction of ineffective effort due to dyssynchrony in ventilated neuromuscular patients and the improvement of sleep parameters [20]. In addition, a higher inspiratory load due to an increase in upper airway resistance and mouth leaks may contribute to the inability to trigger the ventilator [20]. Therefore, the objective of a “volume guarantee” module should not only target the maintenance of a minimal V t during a changes in respiratory system impedance or mouth leaks, but also the maintenance of an accurate patient-ventilator synchronization.
The “volume guarantee” module is based on the measurement of the expired V t. This method has some limits considering that leaks may also occur during expiration and therefore this method may underestimate the real V t [6]. When the expired volume detected by the ventilator is below the minimal desired V t, the ventilator increases its IPAP to reach to minimal target V t. A longer T i could also contribute to increased V t as observed with some of the ventilators tested in this study [17]. A combination of a moderate increase in both IPAP and T i could have the same efficacy with improved patient comfort, as we observed in a pilot study (unpublished data).
Of note, no difference was observed between the results obtained with a simple or a double circuit. This is perfectly understandable in the absence of leaks. In the presence of leaks, all the ventilators that were tested with both a double and a simple circuit failed to deliver a V t because of the systematic occurrence of autotriggering. Therefore, we cannot conclude that a double circuit, when available, outperforms a simple circuit. In addition, the two ventilators that were able to compensate the fall in V t in case of leaks had a simple circuit. This is not in accordance with the principle that a volume guarantee module relies on the automatic detection of the expired V t by the ventilator. In fact, these two ventilators account for leak by adjusting a mathematical leak model as a function of mask pressure, based on the fact that the long-term average of flow into the patient is approximately zero. This model is used to estimate the instantaneous leak and instantaneous mask vent flow (which is a known function of instantaneous mask pressure), which are subtracted from the total flow generator outflow (which is directly measured) to calculate respiratory flow, V t, and ventilation. This method also explained that the inspiratory trigger was not affected with these two ventilators.
The V t indicated by the ventilator was underestimated in the baseline condition in four of the six tested devices (see online supplement). This observation should be taken into account by the clinician during the setting of the “volume guarantee” module. For example, rather than choosing a fixed volume, the setting of a percentage of the indicated V t obtained during a baseline, stable condition may be chosen to set the “volume guarantee.”
In conclusion, the aim of a “volume guarantee” module is to combine greater efficacy of NPPV with improved tolerance. This bench study reveals problems that may occur during NPPV, even in ventilators having “sophisticated” options. The large variations in IPAP and V t, associated with patient ventilator dyssynchrony, may cause poor sleep quality, discomfort, and NPPV intolerance.
References
Navajas D, Farre R, Rotger MM, Milic-Emili J, Sanchis J (1988) Effect of body posture on respiratory impedance. J Appl Physiol 64:194–199
Gonzalez J, Sharshar T, Hart N, Chadda K, Raphael JC, Lofaso F (2003) Air leaks during mechanical ventilation as a cause of persistent hypercapnia in neuromuscular disorders. Intensive Care Med 29:596–602
Rabec C, Georges M, Kabeya NK, Baudouin N, Massin F, Reybet-Degat O, Camus P (2009) Evaluating noninvasive ventilation using a monitoring system coupled to a ventilator: a bench-to-bedside study. Eur Respir J 34:902–913
Lofaso F, Desmarais G, Leroux K, Zalc V, Fodil R, Isabey D, Louis B (2006) Bench evaluation of flow limitation detection by automated continuous positive airway pressure devices. Chest 130:343–349
Fauroux B, Leroux K, Desmarais G, Isabey D, Clément A, Lofaso F, Louis B (2008) Performance of ventilators for noninvasive positive-pressure ventilation in children. Eur Respir J 31:1300–1307
Andrieu MC, Quentin C, Orlikowski D, Desmarais G, Isabey D, Louis B, Lofaso F (2008) Inductive plethysmography to control volume-targeted ventilation for leak compensation. Intensive Care Med 34:1150–1155
Paiva R, Krivec U, Aubertin G, Cohen E, Clément A, Fauroux B (2009) Carbon dioxide monitoring during long-term noninvasive respiratory support in children. Intensive Care Med 35:1068–1074
Storre JH, Seuthe B, Fiechter R, Milioglou S, Dreher M, Sorichter S, Windisch W (2006) Average volume-assured pressure support in obesity hypoventilation: a randomized crossover trial. Chest 130:815–821
Janssens JP, Metzger M, Sforza E (2009) Impact of volume targeting on efficacy of bi-level non-invasive ventilation and sleep in obesity-hypoventilation. Respir Med 103:165–172
Coughlin S, White D (2009) Reply to: Janssens J-P et al., Impact of volume targeting on efficacy of bi-level non-invasive ventilation and sleep in obesity-hypoventilation. Respir Med 103:943
Marrone O, Insalaco G, Bonsignore MR, Romano S, Salvaggio A, Bonsignore G (2002) Sleep structure correlates of continuous positive airway pressure variations during application of an autotitrating continuous positive airway pressure machine in patients with obstructive sleep apnea syndrome. Chest 121:759–767
Meyer TJ, Pressman MR, Benditt J, McCool FD, Millman RP, Natarajan R, Hill NS (1997) Air leaking through the mouth during nocturnal nasal ventilation: effect on sleep quality. Sleep 20:561–569
Teschler H, Stampa J, Ragette R, Konietzko N, Berthon-Jones M (1999) Effect of mouth leak on effectiveness of nasal bilevel ventilatory assistance and sleep architecture. Eur Respir J 14:1251–1257
Fanfulla F, Delmastro M, Berardinelli A, Lupo ND, Nava S (2005) Effects of different ventilator settings on sleep and inspiratory effort in patients with neuromuscular disease. Am J Respir Crit Care Med 172:619–624
Toublanc B, Rose D, Glérant JC, Francois G, Mayeux I, Rodenstein D, Jounieaux V (2007) Assist-control ventilation vs. low levels of pressure support ventilation on sleep quality in intubated ICU patients. Intensive Care Med 33:1148–1154
Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP (2010) Pathophysiology of sleep apnea. Physiol Rev 90:47–112
Orlikowski D, Mroue G, Prigent H, Moulin C, Bohic M, Ruquet M, Raphael JC, Annane D, Lofaso F (2009) Automatic air-leak compensation in neuromuscular patients: a feasibility study. Respir Med 103:173–179
Jaye J, Chatwin M, Dayer M, Morrell MJ, Simonds AK (2009) Autotitrating versus standard noninvasive ventilation: a randomised crossover trial. Eur Respir J 33:566–571
Midgren B (2009) Assisted ventilation during sleep: improving respiration or sleep or both? Respir Med 103:163–164
Fanfulla F, Taurino AE, Lupo ND, Trentin R, D’Ambrosio C, Nava S (2007) Effect of sleep on patient/ventilator asynchrony in patients undergoing chronic non-invasive mechanical ventilation. Respir Med 101:1702–1707
Acknowledgments
The research of Brigitte Fauroux is supported by the Association Française contre les Myopathies (AFM), Assistance Publique-Hôpitaux de Paris, Inserm, Legs Poix, ADEP Assistance, and Université Pierre et Marie Curie-Paris 6.
Conflict of interest statement
All the authors declare that they have no conflict of interest with the data presented in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fauroux, B., Leroux, K., Pépin, JL. et al. Are home ventilators able to guarantee a minimal tidal volume?. Intensive Care Med 36, 1008–1014 (2010). https://doi.org/10.1007/s00134-010-1785-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1785-9