Abstract
Purpose
Lymphangioleiomyomatosis (LAM) is a rare, progressive, frequently lethal cystic lung disease that almost exclusively affects women. Prognostic information in LAM has been limited by small numbers and heterogeneous study methodology. Early retrospective cohorts cited 5- and 10-year mortality of 40 and 80 %, respectively. More recently, mortality at 10 years has been estimated to be approximately 10–20 % from the onset of symptoms and 30 % at 10 years from the time of lung biopsy but varies widely in individual patients. Given the heterogeneous disease course, it would be useful to establish which clinical characteristics are associated with survival to develop prediction models for disease outcome.
Methods
The LAM Foundation maintains a population-based registry of 1,149 registered self-identified LAM patients. Of these, 590 have completed a “General Information/Clinical History Questionnaire” with limited demographic and clinical data, 410 of whom were identified as U.S. residents and provided date of birth. Vital status was obtained on all 410 participants through December 31, 2007 by linking patient identifiers and the National Death Index. Survival time was calculated as the time since first lung-related symptom or physician diagnosis until censoring (still alive, received lung transplant, or died). Cox proportional hazard analysis evaluated the association of demographic and clinical features with survival.
Results
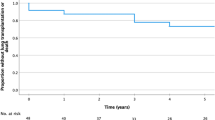
Among the 410 subjects, there were 50 deaths and 55 lung transplantations during a median of 10.4 years of observation time. The estimated median transplant-free survival time for LAM patients in the United States is 29 years from symptom onset and 23 years from diagnosis. The estimated 10-year survival transplant-free was 86 %. Age at disease onset, smoking status, race, presence of tuberous sclerosis, occurrence of pneumothorax, and pregnancy did not demonstrate an association with survival or transplant. Greater age at presentation and presence of angiomyolipoma were associated with less risk of mortality. Treatment with hormonal therapy was associated with an increased risk of death/transplant (hazard ratio (HR) 2.93; 95 % confidence interval (CI), 1.54–5.58; p = 0.001), particularly progesterone therapy (HR 2.17; 95 % CI 1.26–3.75, p = 0.005), and may represent confounding by indication. Patients who required oxygen therapy had a worse outcome (HR 4.53; 95 % CI 2.76–7.42; p < 0.001).
Conclusions
Our population-based study showed that the median survival in patients with LAM from the onset of symptoms or diagnosis is much longer than previously described. This has important implications for life choices and treatment decisions regarding medication use and lung transplantation for patients with LAM.






Similar content being viewed by others
References
Juvet SC, McCormack FX, Kwiatkowski DJ, Downey GP (2007) Molecular pathogenesis of lymphangioleiomyomatosis: lessons learned from orphans. Am J Respir Cell Mol Biol 36(4):398–408
Ryu JH, Moss J, Beck GJ et al (2006) The NHLBI lymphangioleiomyomatosis registry: characteristics of 230 patients at enrollment. Am J Respir Crit Care Med 173(1):105–111
Crino PB, Nathanson KL, Henske EP (2006) The tuberous sclerosis complex. N Engl J Med 355(13):1345–1356
McCormack FX, Inoue Y, Moss J et al (2011) Efficacy and safety of sirolimus in lymphangioleiomyomatosis. N Engl J Med 364(17):1595–1606
O’Callaghan FJ, Noakes MJ, Martyn CN, Osborne JP (2004) An epidemiological study of renal pathology in tuberous sclerosis complex. BJU Int 94(6):853–857
Costello LC, Hartman TE, Ryu JH (2000) High frequency of pulmonary lymphangioleiomyomatosis in women with tuberous sclerosis complex. Mayo Clin Proc 75(6):591–594
Franz DN, Bissler JJ, McCormack FX (2010) Tuberous sclerosis complex: neurological, renal and pulmonary manifestations. Neuropediatrics 41(5):199–208
McCormack FX (2008) Lymphangioleiomyomatosis: a clinical update. Chest 133(2):507–516
Almoosa KF, Ryu JH, Mendez J et al (2006) Management of pneumothorax in lymphangioleiomyomatosis: effects on recurrence and lung transplantation complications. Chest 129(5):1274–1281
Corrin B, Liebow AA, Friedman PJ (1975) Pulmonary lymphangiomyomatosis: a review. Am J Pathol 79(2):348–366
Silverstein EF, Ellis K, Wolffe M, Jaretzki A (1974) Pulmonary lymphangiomyomatosis. Am J Radiol 120:832–850
Johnson SR, Whale CI, Hubbard RB et al (2004) Survival and disease progression in UK patients with lymphangioleiomyomatosis. Thorax 59(9):800–803
Urban T, Lazor R, Lacronique J et al (1999) Pulmonary lymphangioleiomyomatosis. A study of 69 patients. Groupe d’Etudes et de Recherche sur les Maladies “Orphelines” Pulmonaires (GERM”O”P). Medicine (Baltimore) 78(5):321–337
Matsui K, Beasley MB, Nelson WK et al (2001) Prognostic significance of pulmonary lymphangioleiomyomatosis histologic score. Am J Surg Pathol 25(4):479–484
Ho TB, Hull JH, Hughes NC (2006) An 86-year-old female with lymphangioleiomyomatosis. Eur Respir J 28(5):1065
Moses MA, Harper J, Folkman J (2006) Doxycycline treatment for lymphangioleiomyomatosis with urinary monitoring for MMPs. N Engl J Med 354(24):2621–2622
Kitaichi M, Nishimura K, Itoh H, Izumi T (1995) Pulmonary lymphangioleiomyomatosis: a report of 46 patients including a clinicopathologic study of prognostic factors. Am J Respir Crit Care Med 151(2 Pt 1):527–533
Taveira-DaSilva AM, Steagall WK, Rabel A et al (2009) Reversible airflow obstruction in lymphangioleiomyomatosis. Chest 136(6):1596–1603
Taveira-DaSilva AM, Stylianou MP, Hedin CJ et al (2004) Decline in lung function in patients with lymphangioleiomyomatosis treated with or without progesterone. Chest 126(6):1867–1874
Hayashida M, Seyama K, Inoue Y et al (2007) The epidemiology of lymphangioleiomyomatosis in Japan: a nationwide cross-sectional study of presenting features and prognostic factors. Respirology 12(4):523–530
Steagall WK, Glasgow CG, Hathaway OM et al (2007) Genetic and morphologic determinants of pneumothorax in lymphangioleiomyomatosis. Am J Physiol Lung Cell Mol Physiol 293(3):L800–L808
Young LR, Almoosa KF, Pollock-Barziv S et al (2006) Patient perspectives on management of pneumothorax in lymphangioleiomyomatosis. Chest 129(5):1267–1273
Kinder BW, Sherman AC, Young LR et al (2010) Predictors for clinical trial participation in the rare lung disease lymphangioleiomyomatosis. Respir Med 104(4):578–583
Vittinghoff E, Glidden DV, Shiboski SC, McCulloch CE (2005) Regression methods in biostatistics: linear, logistic, survival, and repeated measures models, 1st edn. Springer Science and Business Media, New York
Cohen MM, Freyer AM, Johnson SR (2009) Pregnancy experiences among women with lymphangioleiomyomatosis. Respir Med 103(5):766–772
Celli BR, Cote CG, Marin JM et al (2004) The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 350(10):1005–1012
Acknowledgments
The project described was supported by a University of Cincinnati Dean’s Scholars Grant for Clinical Research; Award Number K23HL094532 and a NIH Clinical Research Loan Repayment Grant (BWK) from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, And Blood Institute or the National Institutes of Health.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oprescu, N., McCormack, F.X., Byrnes, S. et al. Clinical Predictors of Mortality and Cause of Death in Lymphangioleiomyomatosis: A Population-based Registry. Lung 191, 35–42 (2013). https://doi.org/10.1007/s00408-012-9419-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-012-9419-3