Abstract
Objectives
The main aim of this study was to find the prevalence of mortality among hospitalized COVID-19 infected patients and associated risk factors for death.
Methods
Three electronic databases including PubMed, Science Direct and Google Scholar were searched to identify relevant cohort studies of COVID-19 disease from January 1, 2020, to August 11, 2020. A random-effects model was used to calculate pooled prevalence rate (PR), risk ratio (RR) and 95% confidence interval (CI) for both effect measures. Cochrane chi-square test statistic Q, \({I}^{2}\), and \({\tau }^{2}\) tests were used to measure the presence of heterogeneity. Publication bias and sensitivity of the included studies were also tested.
Results
In this meta-analysis, a total of 58 studies with 122,191 patients were analyzed. The pooled prevalence rate of mortality among the hospitalized COVID-19 patients was 18.88%, 95% CI (16.46–21.30), p < 0.001. Highest mortality was found in Europe [PR 26.85%, 95% CI (19.41–34.29), p < 0.001] followed by North America [PR 21.47%, 95% CI (16.27–26.68), p < 0.001] and Asia [PR 14.83%, 95% CI (12.46- 17.21), p < 0.001]. An significant association were found between mortality among COVID-19 infected patients and older age (> 65 years vs. < 65 years) [RR 3.59, 95% CI (1.87–6.90), p < 0.001], gender (male vs. female) [RR 1.63, 95% CI (1.43–1.87), p < 0.001], ICU admitted patients [RR 3.72, 95% CI (2.70–5.13), p < 0.001], obesity [RR 2.18, 95% CI (1.10–4.34), p < 0.05], hypertension [RR 2.08,95% CI (1.79–2.43) p < 0.001], diabetes [RR 1.87, 95% CI (1.23–2.84), p < 0.001], cardiovascular disease [RR 2.51, 95% CI (1.20–5.26), p < 0.05], and cancer [RR 2.31, 95% CI (1.80–2.97), p < 0.001]. In addition, significant association for high risk of mortality were also found for cerebrovascular disease, COPD, coronary heart disease, chronic renal disease, chronic liver disease, chronic lung disease and chronic kidney disease.
Conclusion
This meta-analysis revealed that the mortality rate among COVID-19 patients was highest in the European region and older age, gender, ICU patients, patients with comorbidity had a high risk for case fatality. Those findings would help the health care providers to reduce the mortality rate and combat this pandemic to save lives using limited resources.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by the most recently discovered RNA virus named coronavirus, formerly referred to as severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) [1]. It causes tract infections within the human and animal bodies present with fever, cough, cold, and sometimes patients may die due to acute respiratory distress syndrome or pneumonia [2]. Coronaviruses are a beta coronavirus that constitutes the subfamily Orthocoronavirinae, and family Coronaviridae. The name “coronavirus” is derived from Latin word corona, meaning as crown or wreath. Coronaviruses were first discovered in the 1930s in North Dakota with an acute respiratory tract infection of domesticated chickens [1]. Among seven coronavirus species that are identified to infect human beings and cause disease, HCoV-229E, HCoV-OC43, HCoV-NL63, and HCoV-HKU1 are generally mild, often cause normal cold side effects. Other three human coronaviruses, middle east respiratory syndrome-related coronavirus (MERS-CoV), severe acute respiratory syndrome coronavirus (SARS-CoV), severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) produce potentially severe symptoms, which have been identified in 2012, 2002 and 2019 respectively [3, 4].
The first case of COVID-19 disease was identified on December 8, 2019, in Wuhan, the Hubei province of China by the Chinese Center for Disease and Prevention from the throat swab of a patient [5]. Since COVID-19 disease emergence first in China, it’s rapidly become a worldwide threat and it’s declared as a pandemic by World Health Organization (WHO). From that time, this disease has spread to 216 countries and territories around the world, with 20,995,433 confirmed cases and 760,774 deaths (World Health Organization statistics as on August 15, 2020) [6]. The case fatality rate is high for COVID-19 infection. Globally the death rate was 3.6% [6]. The highest confirmed number of cases was reported in the United States of America with 5,150,407 confirmed cases with 164,826 deaths. From the European region, the majority of confirmed cases/death was accounted from the Russian Federation, Spain, UK, Italy (912,823/15,498, 337,334/28 605, 313,802/46 706, 252,235/35 231) respectively. In the African region, the highest confirmed cases/death was found in South Africa (572,865/11 270) and in the Eastern Mediterranean region highest cases/death was found in Iran (336,324/19 162). From the South-East Asia region, India accounted for the highest number of cases/death (2,461,190/64 553). In Bangladesh, the confirmed number of cases was 269,115 with 3 557 deaths up to August 15, 2020 [6].
Patients with COVID-19 present primarily with various symptoms like fever, cough, dyspnea, myalgia, and fatigue [7, 8]. Although most of the COVID-19 infected patients are thought to be recovered after few days, male patients, older patients (age greater than 60 years) and patients with various chronic diseases may have fetal outcomes [9].
Several factors are responsible for the severity and mortality of COVID-19 disease. From different studies, it had been found that patients with comorbidities such as hypertension, diabetes mellitus, acute respiratory distress syndrome (ARDS), cardiovascular disease, cancer, COPD, asthma, renal disease, kidney disease, liver disease, hepatic disease, pneumonia, obesity, and also for the history of smoking were responsible for the development of the disease or death [10,11,12,13,14]. The mortality rate of COVID-19 patients were varied among the intensive care unit (ICU) and non-ICU patients and also for severe and non-severe patients. From different studies, it had been found that the mortality rate was higher among ICU admitted patients and severe patients compared to non-ICU and non-severe patients [15,16,17].
Low and middle-income countries like Bangladesh, COVID-19 disease is sort of a threat to health and economic sectors. Proper social distancing is not possible for a large number of populations, which is essential to prevent this disease because of having no proper treatment or medicine to treat coronavirus infected patients and vaccine to prevent it. Numerous requiring ICU care and mechanical ventilator, which is difficult to arrange for many developing countries [18]. Proper steps should be taken to prevent this disease and reduce the mortality rate. Several studies had reported the risk factors associated with death among COVID-19 patients [10,11,12,13,14]. In this study, we aimed to review the prevalence of mortality and the risk factors associated with mortality among coronavirus infected patients in the hospital and to summarize the available findings in a meta-analysis.
Methods
Search Strategy
A systematic search had been performed using the online databases of PubMed, Science Direct and Google Scholar for relevant publications from January 1, 2020, to August 11, 2020. Advanced search strategy with the following combined text heading as (“coronavirus” OR “COVID-19” OR “novel coronavirus” OR “SARS-CoV-2” OR “2019-nCoV” OR “Severe Acute Respiratory Syndrome related coronavirus”) AND (“mortality” OR “death” OR “fatal outcome”) AND (“risk factors”) had been used to find out the potential paper. An initial search had been carried out followed by an analysis of the text words contained in Title/Abstract. A literature search had been done by two independent reviewers (FMN and MMI).
Study Eligibility Criteria
We included the articles assessing the association between age, gender, comorbidities and mortality risk factors from COVID-19 infection as the major outcomes of interest. Articles that reported SARS-CoV-2 infected patients confirmed by real time reverse transcriptase polymerase chain reaction (RT-PCR) were included. Studies that didn’t report the prevalence of mortality among COVID-19 patients were excluded. For this analysis purpose, studies with only cohort study design were used. Randomized controlled trials, cross-sectional study, case–control study and case report study design were excluded. Editorials, systematic review articles, letters to editors and short communication were also excluded for this analysis. Studies that included only pediatric patients, pregnant women, surgery patients and patient co-infection with other diseases were excluded due to heterogeneous results found among those groups for coronavirus disease. Articles were written in English language and only human based studies were included. Only published and peer reviewed articles were included in the analysis. Unpublished articles were excluded due to data uncertainty. All the identified articles were investigated by hand and not recognized by electronic inquiry. Duplicate articles were found out and extracted at last. Titles and abstracts were searched by two independent researchers. Controversial matters were resolved after discussion.
Data Extraction Process and study Quality Assessment
Two reviewers independently screened full articles after an initial search by title and abstract for inclusion and exclusion criteria. The extracted data included: confirmation of SARS-CoV-2 infected patients, study design, time and place of data collections, author name, year of publication, country, the total number of reported cases, the total number of fatality cases, gender, age, comorbidities (e. g., hypertension, diabetes, cardiovascular disease, etc.). The results of this analysis were presented based on the PRISMA checklist [19]. Newcastle–Ottawa technique was used for the quality assessment of the included cohort studies [20]. Three major components were utilized to assess the quality of the included studies such as selection procedure of the study patients, coordination of efficient confounding variables and assessment of the outcome and the article’s point with more than 5 were considered as high-quality publications among maximum 9 points [21].
Statistical Analysis
Data analysis was carried out using STATA version 16 and Microsoft Excel. The pooled prevalence rate (PR), risk ratio (RR) and 95% confidence interval (CI) for both of those were calculated using random effects model to pool weighted effect size as well as every individual study. PR was used to calculate the prevalence of mortality among hospitalized patients with COVID-19 and RR was used to calculate the risk of mortality. Random effects model was used in this analysis as there was substantial heterogeneity among the study results. In meta-analysis a random effects model assumes that the effect size of all studies is not uniform and may follow a distribution [22, 23]. For examining the between-study heterogeneity, chi-square test statistic (Q), and \({I}^{2}\) and \({\tau }^{2}\) test were used in this analysis [23, 24]. Forest plot was used as a graphical representation of heterogeneity among the included studies. Substantive heterogeneity among the included studies result was identified by subgroup analysis based on continent. A sensitivity analysis was conducted to find the effect of a single study on the overall study result. Publication bias was detected by funnel plot [25].
Results
Search Results and Study Characteristics
A total of 2147 articles were identified from three databases PubMed, Science Direct and Google Scholar. After screening those articles by title and abstract, 340 articles were identified. Of those, 144 articles were selected for full text assessment. Among those, 58 articles with 122,191 participants reporting the mortality rate and risk factors of mortality among hospitalized patients with confirmed COVID-19 infection as a primary outcome were included. Rest of the 86 articles were excluded due to lack of proper information, study design and duplication. Finally, 58 cohort studies were included in this meta-analysis (Fig. 1). The characteristics of all the included studies were described in (Table 1).
Among the included studies, 26 studies were conducted in China [10,11,12,13, 26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47], 8 in USA [48,49,50,51,52,53,54,55], 7 in Italy [16, 56,57,58,59,60,61], 4 in Spain [14, 62,63,64], 2 in South Korea [65, 66], 2 in Mexico [67, 68], 1 in Bangladesh [69], 1 in Brazil [70], 1 in England [71], I in Greece [72], 1 in Iran [73], 1 in Kuwait [74], 1 in Switzerland [75], 1 in Turkey [76] and 1 in few European countries [77]. The sample size of the included studies varied from 16 to 51,633 patients and the mean age of the included patients varied from 41 years to 85.5 years. Prevalence of mortality among hospitalized coronavirus patients was reported in 58 studies and the risk of mortality was reported in 48 studies. The mortality rate among hospitalized patients varied from 0.6 to 61.5%.
Prevalence of Mortality Among Coronavirus Patients
Summary of this meta-analysis for the prevalence of mortality among hospitalized coronavirus patients and subgroup analysis with respect to continent were presented in Table 2. Total 58 studies with 122,191 patients were used to find the mortality rate. The prevalence of mortality among the hospitalized patients with COVID-19 disease was 18.88%, 95% CI (16.46–21.30), z = 15.30, p < 0.001 (Fig. 2). The subgroup analysis by continent revealed that the mortality of hospitalized patients with COVID-19 was the highest in Europe [PR 26.85%, 95% CI (19.41–34.29), z = 7.07, p < 0.001, \({\tau }^{2}\)= 199.87, \({I}^{2}\)=99.1%] followed by North America [PR 21.47%, 95% CI (16.27–26.68), z = 8.08, p < 0.001, \({\tau }^{2}\)=68.28, \({I}^{2}\)=99.5%], Asia [PR 14.83%, 95% CI (12.46–17.21), z = 12.25, p < 0.001, \({\tau }^{2}\)= 42.14, \({I}^{2}\)=98.8%] and South America [PR 6.33%, 95% CI (5.28- 7.38), z = 11.83, p < 0.001] (Fig. S1).
Risk Factors of Mortality Among Coronavirus Patients
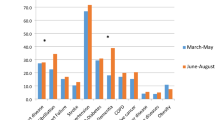
Risk of mortality among hospitalized COVID-19 patients is highly influenced by older age, male patients and patients with different comorbidities. Risk ratio (RR) was used as an effect measure to find the associated risk of mortality among hospitalized COVID-19 patients. Summary of this meta-analysis for the risk of mortality among COVID-19 patients were presented in Table 3. Among 58 studies, 48 studies with 60,623 patients were analyzed to get risk factors for mortality. Mortality among hospitalized COVID-19 patients with age > 65 years were 3.59 times more likely or 259% higher as compared to the patients with age < 65 years [RR 3.59, 95% CI (1.87–6.90), z = 3.84, p < 0.001] (Fig. S2). The risk of mortality among male patients with COVID-19 was 63% higher compared to female patients [RR 1.63, 95% CI (1.43–1.87), z = 7.15, p < 0.001] (Fig. S3). ICU admitted patients with COVID-19 was 3.7 times more likely to die compared to non-ICU patients [RR 3.72 (2.70–5.13), z = 8.01, p < 0.001] (Fig. S4).The risk of mortality among obese patients with COVID-19 was 118% higher compared to non-obese patients [RR 2.18, 95% CI (1.10–4.34), z = 2.22, p < 0.05] (Fig. S5). Mortality among COVID-19 patients with the history of smoking was 81% higher compared to the patients without the history of smoking [RR 1.81, 95% CI (0.99–3.33), z = 1.91, p < 0.1] (Fig. S6). Patients with hypertension was two times as high as patients with no hypertension to die [RR 2.08, 95% CI (1.79–2.43), z = 9.33, p < 0.001] (Fig. S7). Mortality among hospitalized COVID-19 patients with diabetes was 87% higher compared to the patients without diabetes [RR 1.87, 95% CI (1.23–2.84), z = 2.93, p < 0.001] (Fig. S8). The risk of mortality among the patients with cardiovascular disease was 2.5 times more likely than compared to the patients without cardiovascular disease [RR 2.51, 95% CI (1.20–5.26), z = 2.34, p < 0.05] (Fig. S9). Mortality of COVID-19 patients with cerebrovascular disease increased the risk by 165% compared to the patients without cerebrovascular disease [RR 2.75, 95% CI (1.54–4.89), z = 3.44, p < 0.01] (Fig. S10). Patients with asthma was two times as high as the patients without asthma to die due to COVID-19 disease [RR 1.96, 95% CI (0.89–4.33), z = 1.66, p < 0.01] (Fig. S11). Those patients with COPD was two times more likely to die compared to the patients with no COPD [RR 2.23, 95% CI (1.17–4.24), z = 2.44, p < 0.05] (Fig. S12). The risk of mortality was 131% higher among the hospitalized COVID-19 patients with cancer compared to the patients who have no cancer [RR 2.31, 95% CI (1.80–2.97), z = 6.51, p < 0.001] (Fig. S13). The risk of mortality among the hospitalized patients with coronary heart disease [RR 3.63, 95% CI (1.52–8.65), z = 2.90, p < 0.01] (Fig. S14), chronic renal disease [RR 3.82, 95% CI (2.17–6.73), z = 4.64, p < 0.01] (Fig. S15), chronic liver disease [RR 2.02, 95% CI (1.16–3.50), z = 2.48, p < 0.05] (Fig. S16), chronic kidney disease [RR 2.11, 95% CI (1.72–2.58), z = 7.22, p < 0.001] (Fig. S17), chronic lung disease [RR 2.22, 95% CI (1.47–3.35), z = 3.80, p < 0.001] (Fig. S18) were 263%, 282%, 102%, 111% and 122% higher compared to the patients without those disease respectively.
Forest plot was used as a graphical representation of heterogeneity among the study results (Fig. 2, Fig. S1–S18). The overall effect was represented by diamond and individual study effects were represented by squares with their respective 95% CI.
Sensitivity Analysis and Publication Bias
Sensitivity analysis was conveyed to identify the most influential study on the pooled summary effect and risk factors. From sensitivity analysis, it was found that the overall estimates and association of risk factors with COVID-19 mortality did not depend on a single study (Fig. S20–S21). Publication bias was detected by the funnel plot. Most of the variables showed evidence of publication bias (Fig. S19).
Discussion
From this meta-analysis, it had been found that the pooled prevalence of mortality among hospitalized COVID-19 patients was 18.88%. Subgroup analysis was conducted concerning for continent to find out the reason of variation among the mortality rate of COVID-19 patients due to geographical location. The highest mortality was found in Europe followed by North America and Asia. During this this meta-analysis, it was also found that older patients (> 65 years), male patients, obesity, patients with comorbidities such as hypertension, diabetes, cardiovascular disease, cerebrovascular disease, COPD, cancer, coronary heart disease, chronic renal disease, chronic liver disease, chronic kidney disease and chronic lung disease were significantly associated with the risk of mortality among the hospitalized COVID-19 patients.
Though the case fatality rate of SARS-CoV-2 infection was lower than MERS-CoV and SARS-CoV infection, the total number of cases and death was higher for SARS-CoV-2 compared to MERS-CoV and SARS-CoV infection [78, 79]. From a systematic review, it had been found that the case fatality rate for COVID-19 infected patients was 5.6% compared to SARS (13%) and MERS (35%) infected patients [78].
The highest number of mortality for COVID-19 infection was observed in Europe. Among the the European region, the highest mortality was observed in Italy [16, 61] followed by Spain [63, 64]. The case fatality rate was also highest in USA [54, 55]. Compared to European and American countries, the case fatality rate was low in Asian countries. The mortality rate among COVID-19 patients in Bangladesh was 10% [69] followed by Iran and Kuwait 8.06% and 1.73% respectively [73, 74]. Among the Asian region, the highest mortality was found in China and South Korea [47, 66]. A large variation of prevalence of mortality was found among the Chinese population [13, 27, 32, 36, 41, 42, 47].
From several previous studies, older age was found as a potential risk factor for death among COVID-19 patients [50, 60]. Most of the older patients have several chronic diseases and less body fitness to fight with a viral infection, which may be one of the main reasons for fatal outcomes [60, 80]. Older age was also a risk factor for severity and mortality among SARS and MERS infected patients [81, 82]. Male patients with COVID-19 were more likely to die compared to female patients [35, 40, 55, 64]. Different sexual hormones could also be responsible for it. Mortality among male patients was also high for SARS and MERS infected patients compared to female patients [81, 82].
From this meta-analysis, it was found that obese patients with COVID-19 had a higher risk to die compared to non-obese patients. Consistent results were found from several studies [14, 70, 72]. The history of smoking among COVID-19 patients increased the risk of mortality. From a study, it was found that smokers had a 767% higher risk of mortality as non-smoker [32, 33, 74].
Several comorbidities were also responsible for the risk of mortality among hospitalized COVID-19 patients. Comorbid patients with COVID-19 had a high risk of disease severity, ICU admission, including death [83]. Hypertension was the most common underlining comorbidities among COVID-19 patients and the prevalence of mortality among hypertension patients due to COVID-19 was 58.3% [14, 30, 32, 69]. From our meta-analysis, it had been observed that mortality due to COVID-19 was 108% higher in the hypertension group compared to the non-hypertension group. The second most frequent comorbidity was diabetes and the prevalence of mortality among COVID-19 patients with diabetes was 49% [12, 30, 65, 69, 70]. We also observed that the rate of mortality due to COVID-19 infection among diabetes patients was 2 times as high as the patients with no diabetes.
We observed cardiovascular disease as a risk factor for death among COVID-19 infected patients. The previous data also seems to suggest that patients with cardiovascular disease are more likely to die in coronavirus infection [32, 34, 37, 43, 70]. A high rate of case fatality was found for cerebrovascular disease with 56.6% [70]. The prevalence of mortality among patients with asthma was 9.3% and had a higher risk of death compared to the patients with no asthma [69, 70, 72, 74]. From previous studies, it was found that the case fatality rate was high for hospitalized COVID-19 patients with COPD [30, 39, 69, 74]. The previous data seems to suggest patients with cancer are more prone to severe outcomes of COVID-19, including death [11, 32, 33, 69, 75]. Association between mortality among COVID-19 patients and increased chronic disease such as (cardiac, renal, liver, kidney and lung) were also found from several independent studies [13, 30, 32, 33, 37, 39, 42, 65, 66, 69, 70, 74].
The prevalence of mortality among COVID-19 patients admitted in the intensive care unit (ICU) was very high [13, 14, 37, 40, 60, 70]. From our analysis, it was observed that the case fatality rate was 272% higher for ICU admitted patients compared to non-ICU patients. A limited number of ventilation machines, skilled stuffs, and doctors, critical patients may be the main reason for this high risk of mortality. In developing countries, the number of ICUs are also limited.
The pathogenesis of COVID-19 is still unknown. Severity of the disease may depend on cytokine storms of the patients [84]. Acute respiratory distress syndrome is found at the early stages of COVID-19 infected patients and cytokine can lead to acute respiratory distress syndrome, which is one of the main reasons for fatality among the patients [9].
Findings from this analysis would help the policymakers of health care sectors to develop different strategies, management and stratified the patients according to risk for giving proper treatments and nursing with limited resources.
Limitations
This meta-analysis had some limitations. Articles only published in the English language were included in this analysis. The sample size of some included studies was very small which might not recognize uncommon factors. Biasness and high heterogeneity among the included studies was also found. Some risk factors could not be included due to data insufficiency. Evidence of publication bias was also found in the data. However, included studies showed good quality assessments.
Conclusion
This meta-analysis result revealed that the mortality rate among hospitalized COVID-19 patients was high and male gender, older aged patients, patients presented with comorbidities such as hypertension, diabetes, cardiovascular disease etc were highly associated with the risk of death among them. Those findings would help the health care providers or physicians to notice the risk of high mortality among the COVID-19 infected patients and take proper management strategies in health care sectors to reduce this high mortality rate and also combat this COVID-19 pandemic to save human lives.
References
Coronavirus. https://en.wikipedia.org/wiki/Coronavirus.
Wang, D., Hu, B., Hu, C., et al. (2020). Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA, 323(11), 1061–1069.
Su, S., Wong, G., ShiW, L. J., Lai, A. C. K., Zhou, J., et al. (2016). Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiology, 24, 490–502.
Cui, J., Li, F., & Shi, Z. L. (2019). Origin and evolution of pathogenic coronaviruses. Nature Reviews Microbiology, 17, 181–192.
Wu, Z., & McGoogan, J. M. (2020). Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. Journal of American Medical Association, 323, 1239–1242.
World Health Organization (WHO). https://www.who.int.
Yang, J., Zheng, Y., Gou, X., Pu, K., Chen, Z., Guo, Q., et al. (2020). Prevalence of comorbidities in the novel wuhan coronavirus (COVID-19) infection: A systematic review and meta-analysis. International Journal of Infectious Diseases, 8, 782–792.
Noor, F. M., & Islam, M. M. (2020). Prevalence of clinical manifestations and comorbidities of coronavirus (COVID-19) infection: A meta-analysis. Fortune Journal of Health Sciences, 3, 55–97. https://doi.org/10.26502/fjhs009.
Wu, C., Chen, X., Cai, Y., et al. (2020). Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan China. JAMA Internal Medicine, 180(7), 1–11.
Zhang, J., Wang, X., Jia, X., Li, J., Hu, K., Chen, G., et al. (2020). Risk factors for disease severity, unimprovement, and mortality of COVID-19 patients in Wuhan, China. Clinical Microbiology and Infection, 26, 767–772.
Yu, C., Lei, Q., Li, W., Wang, X., Liu, W., Fan, X., et al. (2020). Clinical characteristics, associated factors, and predicting COVID-19 mortality risk: A retrospective study in wuhan, China. American Journal of Preventive Medicine, 59, 168–175.
Cen, Y., Chen, X., Shen, Y., Zhang, X. H., Lei, Y., Xu, C., et al. (2020). Risk factors for disease progression in mild to moderate COVID-19 patients–a multi-center observational study. Clinical Microbiology and Infection, 26, 1242–1247.
Zhou, F., Yu, T., Du, R., Fan, G., Liu, Y., Liu, Z., et al. (2020). Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. The lancet, 395, 1054–1062.
Rocio, L. G., Alberto, U. R., Paloma, T., Maria, L. L., Angel, R. F., Laura, N., et al. (2020). Interleukin-6-based mortality risk model for hospitalised COVID-19 patients. Journal of Allergy and Clinical Immunology, 6749(20), 31027–31037.
Urra, J. M., Cabrera, C. M., Porras, L., & Ródenas, I. (2020). Selective CD8 cell reduction by SARS-CoV-2 is associated with a worse prognosis and systemic inflammation in COVID-19 patients. Clinical Immunology, 29, 108486.
Grasselli, G., Greco, M., Zanella, A., Albano, G., Antonelli, M., Bellani, G., et al. (2020). Risk factors associated with mortality among patients with COVID-19 in Intensive care units in Lombardy Italy. JAMA Internal Medicine. https://doi.org/10.1001/jamainternmed.2020.3539.
Li, T., Lu, L., Zhang, W., Tao, Y., Wang, L., Bao, J., et al. (2020). Clinical characteristics of 312 hospitalized older patients with COVID-19 in Wuhan, China. Archives of Gerontology and Geriatrics, 15, 104185.
Anwar, S., Nasrullah, M., & Hosen, M. J. (2020). COVID-19 and Bangladesh: Challenges and how to address them. Frontiers in Public Health, 8, 154.
Moher, D., Liberati, A., Tetzlaff, J., The PRISMA group, et al. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLOS Medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Margulis, A. V., Pladevall, M., Riera-Guardia, N., Varas-Lorenzo, C., Hazell, L., Berkman, N. D., et al. (2014). Quality assessment of observational studies in a drug-safety systematic review, comparison of two tools: The newcastle-ottawa scale and the RTI item bank. Clinical Epidemiology, 6, 359. https://doi.org/10.2147/CLEP.S66677.
Parohan, M., Yaghoubi, S., Seraji, A., Javanbakht, M. H., Sarraf, P., & Djalali, M. (2020). Risk factors for mortality in patients with coronavirus disease 2019 (COVID-19) infection: A systematic review and meta-analysis of observational studies. The Aging Male, 5, 1–9.
DerSimonian, R., & Laird, N. (1986). Meta-analysis in clinical trials. Controlled Clinical Trials, 7(3), 177–188. https://doi.org/10.1016/0197-2456(86)90046-2.
Borenstein, M., Hedges, L. V., Higgins, J. P., & Rothstein, H. R. (2011). Introduction to meta-analysis. New York: Wiley.
Higgins, J. P. T., & Thompson, S. G. (2002). Quantifying heterogeneity in a meta-analysis. Journal of Statistics in Medicine, 21(11), 1539–1558. https://doi.org/10.1002/sim.1186.
Sutton, A. J., Abrams, K. R., Jones, D. R., Sheldon, T. A., & Song, F. (2000). Methods for meta-analysis in medical research. Chichester: Wiley.
Deng, X., Yang, J., Wang, W., Wang, X., Zhou, J., Chen, Z., et al. (2020). Case fatality risk of the first pandemic wave of novel coronavirus disease 2019 (COVID-19) in China. Clinical Infectious Diseases, 13, 199–203.
Chen, R., Liang, W., Jiang, M., Guan, W., Zhan, C., Wang, T., et al. (2020). Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest, 158, 97–105.
Hou, W., Zhang, W., Jin, R., Liang, L., Xu, B., & Hu, Z. (2020). Risk factors for disease progression in hospitalized patients with COVID-19: A retrospective cohort study. Infectious Diseases, 5, 1–8.
Zhang, Y., Cui, Y., Shen, M., Zhang, J., Liu, B., Dai, M., et al. (2020). Association of diabetes mellitus with disease severity and prognosis in COVID-19: A retrospective cohort study. Diabetes Research and Clinical Practice, 165, 108227.
Wang, K., Zuo, P., Liu, Y., Zhang, M., Zhao, X., Xie, S., et al. (2020). Clinical and laboratory predictors of in-hospital mortality in patients with COVID-19: A cohort study in Wuhan, China. Clinical Infectious Diseases, 10, ciaa538.
Chen, J., Bai, H., Liu, J., Chen, G., Liao, Q., Yang, J., et al. (2020). Distinct clinical characteristics and risk factors for mortality in female COVID-19 inpatients: A sex-stratified large-scale cohort study in Wuhan, China. Clinical Infectious Diseases, 8, ciaa920.
Yao, Q., Wang, P., Wang, X., Qie, G., Meng, M., Tong, X., et al. (2020). A retrospective study of risk factors for severe acute respiratory syndrome coronavirus 2 infections in hospitalized adult patients. Polish Archives of Internal Medicine, 130(5), 390–399.
Chen, L., Yu, J., He, W., Chen, L., Yuan, G., Dong, F., et al. (2020). Risk factors for death in 1859 subjects with COVID-19. Leukemia, 34(8), 2173–2183.
Du, R. H., Liang, L. R., Yang, C. Q., Wang, W., Cao, T. Z., Li, M., et al. (2020). Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: A prospective cohort study. European Respiratory Journal, 55(5), 524.
Chen, F., Sun, W., Sun, S., Li, Z., Wang, Z., & Yu, L. (2020). Clinical characteristics and risk factors for mortality among inpatients with COVID-19 in Wuhan, China. Clinical and Translational Medicine, 10(2), e40.
Chen, F. F., Zhong, M., Liu, Y., Zhang, Y., Zhang, K., Su, D. Z., et al. (2020). The characteristics and outcomes of 681 severe cases with COVID-19 in China. Journal of Critical Care, 146, NEJMoa2002032.
Shi, Q., Zhang, X., Jiang, F., Zhang, X., Hu, N., Bimu, C., et al. (2020). Clinical characteristics and risk factors for mortality of COVID-19 patients with diabetes in Wuhan, China: A two-center, retrospective study. Diabetes Cares, 43(7), 1382–1391.
Li, X., Xu, S., Yu, M., Wang, K., Tao, Y., Zhou, Y., et al. (2020). Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. Journal of Allergy and Clinical Immunology, 146(1), 110–118.
Wang, L., He, W., Yu, X., Hu, D., Bao, M., Liu, H., et al. (2020). Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up. Journal of Infection, 80(6), 639–645.
Yang, K., Sheng, Y., Huang, C., Jin, Y., Xiong, N., Jiang, K., et al. (2020). Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: A multicentre, retrospective, cohort study. The Lancet Oncology, 21(7), 904–913.
Luo, M., Liu, J., Jiang, W., Yue, S., Liu, H., & Wei, S. (2020). IL-6 and CD8+ T cell counts combined are an early predictor of in-hospital mortality of patients with COVID-19. JCI insight, 5(13), e139024.
Zhao, Y., Nie, H. X., Hu, K., Wu, X. J., Zhang, Y. T., Wang, M. M., et al. (2020). Abnormal immunity of non-survivors with COVID-19: Predictors for mortality. Infectious Diseases of Poverty, 9(1), 1.
Zhang, L., Han, C., Zhang, S., Duan, C., Shang, H., Bai, T., et al. (2020). Diarrhea and altered inflammatory cytokine pattern in severe COVID-19: Impact on disease course and in-hospital mortality. Journal of Gastroenterology and Hepatology, 16(10), 1753–1766.
Chen, X., Yan, L., Fei, Y., & Zhang, C. (2020). Laboratory abnormalities and risk factors associated with in-hospital death in patients with severe COVID-19. Journal of Clinical Laboratory Analysis, 1, e23467.
Cheng, A., Hu, L., Wang, Y., Huang, L., Zhao, L., Zhang, C., et al. (2020). Diagnostic performance of initial blood urea nitrogen combined with D-Dimer levels for predicting in-hospital mortality in COVID-19 patients. International Journal of Antimicrobial Agents, 23, 106110.
Meng, Y., Lu, W., Guo, E., Liu, J., Yang, B., Wu, P., et al. (2020). Cancer history is an independent risk factor for mortality in hospitalized COVID-19 patients: a propensity score-matched analysis. Journal of Hematology and Oncology, 13(1), 1–1.
Xu, J., Yang, X., Yang, L., Zou, X., Wang, Y., Wu, Y., et al. (2020). Clinical course and predictors of 60-day mortality in 239 critically ill patients with COVID-19: A multicenter retrospective study from Wuhan, China. Critical Care, 24(1), 1–1.
Redd, W. D., Zhou, J. C., Hathorn, K. E., McCarty, T. R., Bazarbashi, A. N., Thompson, C. C., et al. (2020). Prevalence and characteristics of gastrointestinal symptoms in patients with severe acute respiratory syndrome coronavirus 2 infection in the United States: A multicenter cohort study. Gastroenterology, 159(2), 765–767.e2.
Mikami, T., Miyashita, H., Yamada, T., Harrington, M., Steinberg, D., Dunn, A., et al. (2020). Risk factors for mortality in patients with COVID-19 in New York city. Journal of General Internal Medicine, 30, 1.
Imam, Z., Odish, F., Gill, I., O'Connor, D., Armstrong, J., Vanood, A., et al. (2020). Older age and comorbidity are independent mortality predictors in a large cohort of 1305 COVID-19 patients in michigan United States. Journal of Internal Medicine. https://doi.org/10.1111/joim.13119.
Hirsch, J. S., Ng, J. H., Ross, D. W., Sharma, P., Shah, H. H., Barnett, R. L., et al. (2020). Acute kidney injury in patients hospitalized with COVID-19. Kidney International, 98(1), 209–218.
Klang, E., Kassim, G., Soffer, S., Freeman, R., Levin, M. A., & Reich, D. L. (2020). Morbid obesity as an independent risk factor for COVID-19 mortality in hospitalized patients younger than 50. Obesity. https://doi.org/10.1002/oby.22913.
Gupta, S., Hayek, S. S., Wang, W., Chan, L., Mathews, K. S., Melamed, M. L., et al. (2020). Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Internal Medicine. https://doi.org/10.1001/jamainternmed.2020.3596.
Cummings, M. J., Baldwin, M. R., Abrams, D., Jacobson, S. D., Meyer, B. J., Balough, E. M., et al. (2020). Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York city: A prospective cohort study. The Lancet, 395(10239), 1763–1770.
Chilimuri, S., Sun, H., Alemam, A., Mantri, N., Shehi, E., Tejada, J., et al. (2020). Predictors of mortality in adults admitted with COVID-19: Retrospective cohort study from New York city. Western Journal of Emergency Medicine, 21(4), 779.
Di Castelnuovo, A., Bonaccio, M., Costanzo, S., Gialluisi, A., Antinori, A., Berselli, N., et al. (2020). Common cardiovascular risk factors and in-hospital mortality in 3894 patients with COVID-19: survival analysis and machine learning-based findings from the multicentre Italian CORIST Study. Nutrition, Metabolism and Cardiovascular Diseases. https://doi.org/10.1093/cvr/cvaa106.
Giacomelli, A., Ridolfo, A. L., Milazzo, L., Oreni, L., Bernacchia, D., Siano, M., et al. (2020). 30-day mortality in patients hospitalized with COVID-19 during the first wave of the Italian epidemic: A prospective cohort study. Pharmacological Research, 22, 104931.
Borghesi, A., Zigliani, A., Golemi, S., Carapella, N., Maculotti, P., Farina, D., et al. (2020). Chest X-ray severity index as a predictor of in-hospital mortality in coronavirus disease 2019: A study of 302 patients from Italy. International Journal of Infectious Diseases. https://doi.org/10.1016/j.ijid.2020.05.021.
Fattizzo, B., Giannotta, J. A., Sciumè, M., Cattaneo, D., Bucelli, C., Fracchiolla, N. S., et al. (2020). Reply to “COVID-19 in persons with haematological cancers”: A focus on myeloid neoplasms and risk factors for mortality. Leukemia, 26, 1–4.
Covino, M., De Matteis, G., Santoro, M., Sabia, L., Simeoni, B., Candelli, M., et al. (2020). Clinical characteristics and prognostic factors in COVID-19 patients aged≥ 80 years. Geriatrics and Gerontology International. https://doi.org/10.1111/ggi.13960.
Bonetti, G., Manelli, F., Patroni, A., Bettinardi, A., Borrelli, G., Fiordalisi, G., et al. (2020). Laboratory predictors of death from coronavirus disease 2019 (COVID-19) in the area of Valcamonica, Italy. Clinical Chemistry and Laboratory Medicine (CCLM). https://doi.org/10.1515/cclm-2020-0459.
Poblador-Plou, B., Carmona-Pírez, J., Ioakeim-Skoufa, I., Poncel-Falcó, A., Bliek-Bueno, K., Cano-del Pozo, M., et al. (2020). Baseline chronic comorbidity and mortality in laboratory-confirmed COVID-19 cases: Results from the PRECOVID study in Spain. International Journal of Environmental Research and Public Health, 17(14), 5171.
Goicoechea, M., Cámara, L. A., Macías, N., de Morales, A. M., Rojas, Á. G., Bascuñana, A., et al. (2020). COVID-19: clinical course and outcomes of 36 hemodialysis patients in Spain. Kidney International, 98(1), 27–34.
Mostaza, J. M., García-Iglesias, F., González-Alegre, T., Blanco, F., Varas, M., Hernández-Blanco, C., et al. (2020). Clinical course and prognostic factors of COVID-19 infection in an elderly hospitalized population. Archives of Gerontology and Geriatrics, 27, 104204.
Lee, J. Y., Kim, H. A., Huh, K., Hyun, M., Rhee, J. Y., Jang, S., et al. (2020). Risk factors for mortality and respiratory support in elderly patients hospitalized with COVID-19 in Korea. Journal of Korean Medical Science. https://doi.org/10.3346/jkms.2020.35.e223.
Hwang, J. M., Kim, J. H., Park, J. S., Chang, M. C., & Park, D. (2020). Neurological diseases as mortality predictive factors for patients with COVID-19: A retrospective cohort study. Neurological Sciences, 8, 1–8.
Remes-Troche, J. M., Ramos-de-la-Medina, A., Manríquez-Reyes, M., Martínez-Pérez-Maldonado, L., Lara, E. L., & Solís-González, M. A. (2020). Initial gastrointestinal manifestations in patients with SARS-CoV-2 in 112 patients from veracruz (Southeastern Mexico). Gastroenterology. https://doi.org/10.1053/j.gastro.2020.05.055.
Bello-Chavolla, O. Y., Bahena-Lopez, J. P., Antonio-Villa, N. E., Vargas-Vázquez, A., González-Díaz, A., Márquez-Salinas, A., et al. (2020). Predicting mortality due to SARS-CoV-2: A mechanistic score relating obesity and diabetes to COVID-19 outcomes in Mexico. MedRxiv. https://doi.org/10.1210/clinem/dgaa346.
Mowla, S. G., Azad, K. A., Kabir, A., Biswas, S., Islam, M. R., Banik, G. C., et al. (2020). Clinical profile of 100 confirmed COVID-19 patients admitted in dhaka medical college hospital, Dhaka, Bangladesh. Journal of Bangladesh College of Physicians and Surgeons, 9, 29–36.
Sousa, G. J., Garces, T. S., Cestari, V. R., Florêncio, R. S., Moreira, T. M., & Pereira, M. L. (2020). Mortality and survival of COVID-19. Epidemiology and Infection. https://doi.org/10.1016/S1473-3099(20)30195-X.
Smith, A. A., Fridling, J., Ibhrahim, D., & Porter, P. S., Jr. (2020). Identifying Patients at Greatest risk of mortality due to COVID-19: A new England perspective. Western Journal of Emergency Medicine, 21(4), 785.
Halvatsiotis, P., Kotanidou, A., Tzannis, K., Jahaj, E., Magira, E., Theodorakopoulou, M., et al. (2020). Demographic and clinical features of critically ill patients with COVID-19 in Greece: The burden of diabetes and obesity. Diabetes Research and Clinical Practice. https://doi.org/10.1016/j.diabres.2020.108331.
Nikpouraghdam, M., Farahani, A. J., Alishiri, G., Heydari, S., Ebrahimnia, M., Samadinia, H., et al. (2020). Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in IRAN: A single center study. Journal of Clinical Virology. https://doi.org/10.1016/j.jcv.2020.104378.
Almazeedi, S., Al-Youha, S., Jamal, M. H., Al-Haddad, M., Al-Muhaini, A., Al-Ghimlas, F., et al. (2020). Characteristics, risk factors and outcomes among the first consecutive 1096 patients diagnosed with COVID-19 in Kuwait. EClinicalMedicine, 4, 100448.
Pellaud, C., Grandmaison, G., Hoa Phong, P. H., Baumberger, M., Carrel, G., Ksouri, H., et al. (2020). Characteristics, comorbidities, 30-day outcome and in-hospital mortality of patients hospitalised with COVID-19 in a Swiss area–a retrospective cohort study. Swiss Medical Weekly. https://doi.org/10.1016/j.ijid.2020.06.099.
Satici, C., Demirkol, M. A., Altunok, E. S., Gursoy, B., Alkan, M., Kamat, S., et al. (2020). Performance of pneumonia severity index and CURB-65 in predicting 30-day mortality in patients with COVID-19. International Journal of Infectious Diseases. https://doi.org/10.1016/j.ijid.2020.06.038.
Garcia, P. D., Fumeaux, T., Guerci, P., Heuberger, D. M., Montomoli, J., Roche-Campo, F., et al. (2020). Prognostic factors associated with mortality risk and disease progression in 639 critically ill patients with COVID-19 in Europe: Initial report of the international RISC-19-ICU prospective observational cohort. EClinicalMedicine. https://doi.org/10.1016/j.eclinm.2020.100449.
Pormohammad, A., Ghorbani, S., Khatami, A., Farzi, R., Baradaran, B., Turner, D. L., et al. (2020). Comparison of confirmed COVID-19 with SARS and MERS cases-clinical characteristics, laboratory findings, radiographic signs and outcomes: A systematic review and meta-analysis. Reviews in Medical Virology, 5, e2112.
Mahase, E. (2020). Coronavirus: Covid-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. The British Medical Journal. https://doi.org/10.1136/bmj.m641.
Iaccarino, G., Grassi, G., Borghi, C., Ferri, C., Salvetti, M., & Volpe, M. (2020). Age and multimorbidity predict death among COVID-19 patients: results of the SARS-RAS study of the Italian Society of hypertension. Hypertension, 76(2), 366–372.
Choi, K. W., Chau, T. N., Tsang, O., The Princess Margaret Hospital SARS Study Group, et al. (2003). Outcomes and prognostic factors in 267 patients with severe acute respiratory syndrome in Hong Kong. Annals of Internal Medicine. https://doi.org/10.7326/0003-4819-139-9-200311040-00005.
Hong, K. H., Choi, J. P., Hong, S. H., et al. (2018). Predictors of mortality in Middle East respiratory syndrome (MERS). Thorax, 73, 286–289.
Guan, W. J., Liang, W. H., Zhao, Y., Liang, H. R., Chen, Z. S., Li, Y. M., et al. (2020). Comorbidity and its impact on 1590 patients with covid-19 in China: A nationwide analysis. European Respiratory Journal. https://doi.org/10.1183/13993003.00547-2020.
Quartuccio, L., Sonaglia, A., McGonagle, D., Fabris, M., Peghin, M., Pecori, D., et al. (2020). Profiling COVID-19 pneumonia progressing into the cytokine storm syndrome: results from a single Italian centre study on tocilizumab versus standard of care. Journal of Clinical Virology., 15, 104444.
Funding
This research has no fund.
Author information
Authors and Affiliations
Contributions
FMN and MMI formulated the research questions, designed the study, developed the search strategy, searched and collected the articles, conducted the quality assessment, analyzed the data and drafted the manuscript. Finally, both authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict of interest.
Ethical Approval
Ethical approval is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Noor, F.M., Islam, M.M. Prevalence and Associated Risk Factors of Mortality Among COVID-19 Patients: A Meta-Analysis. J Community Health 45, 1270–1282 (2020). https://doi.org/10.1007/s10900-020-00920-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-020-00920-x