ABSTRACT
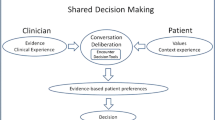
Clinical practice guidelines aim to improve the health of patients by guiding individual care in clinical settings. Many guidelines specifically about health promotion or primary disease prevention are beginning to support informed patient choice, and suggest that clinicians and patients engage in shared discussions to determine how best to tailor guidelines to individuals. However, guidelines generally do not address how to translate evidence from the population to the individual in clinical practice, or how to engage patients in these discussions. In addition, they often fail to reconcile patients’ preferences and social norms with best evidence. Shared decision making (SDM) is one solution to bridge guidelines about health promotion and disease prevention with clinical practice. SDM describes a collaborative process between patients and their clinicians to reach agreement about a health decision involving multiple medically appropriate treatment options. This paper discusses: 1) a brief overview of SDM; 2) the potential role of SDM in facilitating the implementation of prevention-focused practice guidelines for both preference-sensitive and effective care decisions; and 3) avenues for future empirical research to test how best to engage individual patients and clinicians in these complex discussions about prevention guidelines. We suggest that SDM can provide a structure for clinicians to discuss clinical practice guidelines with patients in a way that is evidence-based, patient-centered, and incorporates patients’ preferences. In addition to providing a model for communicating about uncertainty at the individual level, SDM can provide a platform for engaging patients in a conversation. This process can help manage patients’ and clinicians’ expectations about health behaviors. SDM can be used even in situations with strong evidence for benefits at the level of the population, by helping patients and clinicians prioritize behaviors during time-pressured medical encounters. Involving patients in discussions could lead to improved health through better adherence to chosen options, reduced practice variation about preference-sensitive options, and improved care more broadly. However, more research is needed to determine the impact of this approach on outcomes such as morbidity and mortality.
Similar content being viewed by others
REFERENCES
Field MJ, Lohr KN. Clinical Practice Guidelines: Directions for a New Program, Institute of Medicine Committee to Advise the Public Health Service on Clinical Practice Guidelines. Washington: National Academies Press; 1990.
Woolf SH, Grol R, Hutchinson A, Eckles M, Grimshaw J. Clinical guidelines: potential benefits, limitations, and harms of clinical guidelines. BMJ. 1999;318:527–30.
Grimshaw J, Eccles M, Tetroe J. Implementing clinical guidelines: current evidence and future implications. J Contin Educ Health Prof. 2004;24:S31–7.
Grol R. Improving the quality of medical care: building bridges among professional pride, payer profit, and patient satisfaction. JAMA. 2001;286:2578–85.
U.S. Preventive Services Task Force. Screening for Colorectal Cancer: U.S. Preventive Services Task Force Recommendation Statement. Accessed August 1, 2012 from http://www.uspreventiveservicestaskforce.org/uspstf/uspscolo.htm; 2008.
U.S. Preventive Services Task Force. Screening for Breast Cancer: Recommendation Statement. Accessed August 1, 2012 from http://www.uspreventiveservicestaskforce.org/uspstf09/breastcancer/brcanrs.htm; 2009.
Pearson TA, Blair SN, Daniels SR, et al. AHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 Update Consensus Panel Guide to Comprehensive Risk Reduction for Adult Patients Without Coronary or Other Atherosclerotic Vascular Diseases. Circulation. 2002;106:388–91.
U.S. Preventive Services Task Force. Aspirin for the primary prevention of cardiovascular events: recommendations and rationale. Ann Intern Med. 2002;136:157–60.
Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282.
Schunemann HJ, Fretheim A, Oxman AD. Improving the use of research evidence in guideline development: 10. Integrating values and consumer involvement. Health Res Policy Syst. 2006;4.
Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60:301–12.
Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2011;10:CD001431. doi:10.1002/14651858.CD001431.pub3.
Coylewright M, Montori V, Ting HH. Patient-centered shared decision making: a public imperative. Am J Med. 2012;125:545–7.
Elwyn G, Frosch D, Thomson R, et al. Shared Decision Making: A Model for Clinical Practice. 2012;27(10):1361–7.
Mann DM, Ponieman D, Montori VM, et al. The Statin Choice decision aid in primary care: a randomized trial. Patient Educ Couns. 2010;80:138–40.
Decision Laboratory at Cardiff University. Option Grid: High cholesterol. http://www.optiongrid.co.uk/resources/High_cholesterol-Option_Grid.pdf; 2011
United States Office of the Legislative Counsel. Patient Protection and Affordable Care Act. http://docs.house.gov/energycommerce/ppacacon.pdf; 2010.
Elwyn G, Laitner S, Coulter A, et al. Implementing shared decision making in the NHS. BMJ. 2010;341.
Legare F, Stacey D, Forest P-G. Shared decision-making in Canada: update, challenges and where next. Ger J Qual Health Care. 2007;101:213–21.
Street RL. Aiding medical decision making: a communication perspective. Med Decis Making. 2007;27:550–3.
U.S. Preventive Services Task Force. Screening for Prostate Cancer: Recommendation Statement. Accessed July 10, 2012 from http://www.uspreventiveservicestaskforce.org/prostatecancerscreening.htm; 2012.
Wennberg J. Perspective: Practice Variations And Health Care Reform: Connecting The Dots. Health Affairs Web Exclusive: doi:10.1377/hlthaff.var.140; 2004.
Wennberg J. Time to tackle unwarranted variations in practice. BMJ. 2011;342:d1513.
Sirovich B, Gallager PM, Wennberg DE, et al. Discretionary decision making by primary care physicians and the cost of U.S. health care. Heal Aff. 2008;27:813–23.
Evans R, Edwards A, Brett J, et al. Reduction in uptake of PSA tests following decision aids: systematic review of current aids and their evaluations. Patient Educ Couns. 2005;58:13–26.
Politi MC, Han PKJ, Col NF. Communicating the uncertainty of harms and benefits of medical interventions. Med Decis Making. 2007;27:681–95.
Steiner JF. Talking about treatment: the language of populations and the language of individuals. Ann Intern Med. 1999;130:618–22.
Djulbegovic B, Paul A. From efficacy to effectiveness in the face of uncertainty. JAMA. 2011;305:2005–6.
Lewis CL, Golin CE, DeLeon C, et al. A targeted decision aid for the elderly to decide whether to undergo colorectal cancer screening: development and results of an uncontrolled trial. BMC Med Inform Decis Making. 2010;10:54.
Heininger E. A risk–benefit analysis of vaccination. Vaccine. 2009;27:G9–12.
Boivin A, Legare F, Gagnon MP. Competing norms: Canadian rural family physicians’ perceptions of clinical practice guidelines and shared decision-making. J Health Serv Res Policy. 2008;13:79–84.
Johnson CG, Levenkron JC, Suchman AL, et al. Does physician uncertainty affect patient satisfaction? J Gen Intern Med. 1988;3:144–9.
Parascandola M, Hawkins J, Danis M. Patient autonomy and the challenge of clinical uncertainty. Kennedy Inst Ethics J. 2002;12:245–64.
Tosteson AN, Grove MR, Hammond CS, et al. Early discontinuation of treatment for osteoporosis. Am J Med. 2003;115:209–16.
Elwyn G, Frosch D, Rollnick S. Dual equipoise shared decision making: definitions for decision and behaviour support interventions. Implement Sci. 2009;4:75.
O’Connor AM, Bennett C, Stacey D, et al. Do patient decision aids meet effectiveness criteria of the International Patient Decision Aid Standards Collaboration? A systematic review and meta-analysis. Med Decis Making. 2007;27:554–74.
Joosten EAG, DeFuentes-Merillasa L, de Weertc GH, et al. Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother Psychosom. 2008;77:219–26.
Legare F, Ratte S, Gravel K, et al. Barriers and facilitators to implementing shared decision-making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns. 2009;73:526–35.
Legare F, Ratte S, Stacey D, et al. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2010 (Issue 5); doi:10.1002/14651858.CD006732.pub2.
Say R, Murtagh M, Thomson R. Patients’ preference for involvement in medical decision making: a narrative review. Patient Educ Couns. 2006;60:102–14.
Mazur DJ, Hickam DH. Patients’ preferences for risk disclosure and role in decision making for invasive medical procedures. J Gen Intern Med. 1997;12:114–7.
Crawford ED, Bennett CL, Stone NN, et al. Comparison of perspectives on prostate cancer: analyses of survey data. Urology. 1997;50:366–72.
Rockhill B. Theorizing about causes at the individual level while estimating effects at the population level: implications for prevention. Epidemiol Soc. 2005;16:124–9.
Elwyn G, Frosch D, Volandes AE, et al. Investing in deliberation: a definition and classification of decision support interventions for people facing difficult health decisions. Med Decis Making. 2010;30:701–11.
van der Weijden T, Boivin A, Burgers J, et al. Clinical practice guidelines and patient decision aids. An inevitable relationship. J Clin Epidemiol. 2012;65:584–9.
Decision Laboratory at Cardiff University. Option Grids. Accessed July 15, 2012 from http://www.optiongrid.co.uk/; 2009.
Whitney SN, McGuire AL, McCullough LB. A typology of shared decision making, informed consent, and simple consent. Ann Intern Med. 2004;140:54–9.
Drake RE, Deegan PE. Shared decision making Is an ethical imperative. Psychiatr Serv. 2009;60:1009.
Acknowledgements
Contributors
We would like to thank Siobhan Sutcliffe and Rachel Zeuner for their helpful suggestions for improving this manuscript.
Funders
Not applicable
Prior Presentations
Not applicable.
Conflict of Interest
Dr. Politi is on the US Medication Adherence Advisory Board (Merck).
Dr. Wolin is a consultant for Ivynia, LLC.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Politi, M.C., Wolin, K.Y. & Légaré, F. Implementing Clinical Practice Guidelines About Health Promotion and Disease Prevention Through Shared Decision Making. J GEN INTERN MED 28, 838–844 (2013). https://doi.org/10.1007/s11606-012-2321-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-2321-0