Abstract
Benefits of triple therapy with a long-acting muscarinic antagonist (LAMA), added to inhaled corticosteroid (ICS)/long-acting β2-agonist (LABA), have been demonstrated. Limited data assessing the efficacy of the LAMA umeclidinium (UMEC) added to ICS/LABA are available. The aim of this study is to evaluate the efficacy and safety of UMEC added to ICS/LABAs in patients with moderate-to-very-severe COPD. This is a multicentre, randomised, double-blind, parallel-group study. Patients were symptomatic (modified Medical Research Council Dyspnoea Scale score ⩾2), despite receiving ICS/LABA (fluticasone propionate/salmeterol (FP/SAL, branded) 500/50 mcg, budesonide/formoterol (BD/FOR, branded) 200/6 mcg or 400/12 mcg, or other ICS/LABAs) ⩾30 days before the run-in (7±2 days). Patients were randomised 1:1 to once-daily UMEC 62.5 mcg or placebo (PBO), added to twice-daily open-label ICS/LABA for 12 weeks. Primary end point was trough forced expiratory volume in 1 s (FEV1) at Day 85; secondary end point was weighted mean (WM) 0–6 h FEV1 at Day 84; other end points included COPD Assessment Test (CAT) score and Transition Dyspnoea Index (TDI) score. Adverse events (AEs) were investigated. In the UMEC+ICS/LABA and PBO+ICS/LABA groups, 119 and 117 patients were randomised, respectively. Patients received FP/SAL (40%), BD/FOR (43%) and other ICS/LABAs (17%). UMEC+ICS/LABA resulted in significant improvements in trough FEV1 (Day 85) and in WM 0–6 h FEV1 (Day 84) versus PBO+ICS/LABA (difference: 123 and 148 ml, respectively, both P<0.001). Change from baseline for UMEC+ICS/LABA versus PBO+ICS/LABA was significantly different for CAT score at Day 84 (−1.31, P<0.05), but not for TDI score (0.40, P=0.152). AE incidence was similar with UMEC+ICS/LABA (38%) and PBO+ICS/LABA (42%). UMEC+ICS/LABA improved lung function and CAT score in patients with symptomatic COPD versus PBO+ICS/LABA (ClinicalTrials.gov NCT02257372).
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is characterised by persistent airflow limitation, which contributes significantly to morbidity and mortality, and it presents a significant economic burden worldwide.1 Recent estimates predict that COPD will be the third leading cause of death globally by 2030.2 Pharmacologic treatment of COPD is used to reduce symptoms, improve health status and exercise tolerance, and reduce the frequency and severity of exacerbations.1 Triple therapy (the combination of long-acting muscarinic antagonist (LAMA) with inhaled corticosteroid (ICS)/long-acting β2-agonist (LABA)) is recommended as a secondary treatment option in patients experiencing frequent COPD symptoms with a high risk of exacerbations.1 A recent retrospective study assessed trends in management and outcomes of COPD in general practice, including the use of triple therapy.3 The study showed that the use of triple therapy between 2004 and 2009 increased from 10 to 29% in moderate COPD, from 17 to 45% in severe COPD and from 25 to 59% in very severe COPD.3
Umeclidinium (UMEC) is a LAMA for which the 62.5 mcg (delivered dose, 55 mcg) dose has been approved as maintenance therapy for COPD in the US and the EU.4,5 Four Phase III, randomised studies have previously investigated the efficacy and safety of once-daily UMEC 62.5 mcg added to twice-daily fluticasone propionate/salmeterol (FP/SAL) 250/50 mcg or once-daily fluticasone furoate/vilanterol (FF/VI) 100/25 mcg.6,7 Statistically significant and clinically meaningful improvements in trough forced expiratory volume in 1 s (FEV1) were observed for UMEC 62.5 mcg added to FP/SAL 250/50 mcg or added to FF/VI 100/25 mcg compared with placebo (PBO) added to the respective ICS/LABA combinations (122−147 ml; P⩽0.001 for all). In all four studies, UMEC 62.5 mcg added to ICS/LABA was well-tolerated. Post hoc integrated analyses combining all four studies reported positive benefits on patient-reported outcomes (PROs) when using UMEC 62.5 mcg+ICS/LABA compared with PBO+ICS/LABA.8,9
FP/SAL and budesonide/formoterol (BD/FOR) are among the most widely used ICS/LABA combinations.10 Although the prospective data are available on the efficacy of UMEC added to FP/SAL 250/50 mcg7 and FF/VI,6 no studies have investigated the effect of UMEC added to other ICS/LABA combinations such as BD/FOR or the FP/SAL 500/50-mcg dose that is approved in the EU.11 As such, there is a need to determine the effect of UMEC added to other ICS/LABA combinations typically used to treat COPD, including FP/SAL 500/50 mcg and BD/FOR.
The purpose of the current add-on study was to evaluate the efficacy and safety of UMEC 62.5 mcg when added to frequently used ICS/LABA combinations at approved doses in patients with moderate-to-very-severe COPD who remained symptomatic despite receiving unselected ICS/LABA combinations before study entry. We believe that these results will complement and extend the pool of data already available for UMEC+ICS/LABA treatment, thus potentially increasing the generalisability of these data.
Results
Study population
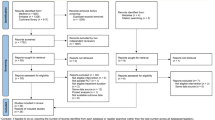
A total of 266 patients were enrolled in the study. After screening, 236 patients were randomised and all were included in the intent-to-treat (ITT) population (Figure 1). A total of 229 patients in the ITT population were included in the per-protocol population. Overall, 219 (93%) patients in the ITT population completed the study (Figure 1).
In the UMEC+ICS/LABA and PBO+ICS/LABA groups, 119 and 117 patients were randomised, respectively, receiving FP/SAL 500/50 mcg (GSK, 40%), BD/FOR (AstraZeneca, 43%) and other ICS/LABA combinations including generics (17%) (Supplementary Table S1).
In terms of baseline characteristics, there was a smaller proportion of current smokers in the UMEC+ICS/LABA group than in the PBO+ICS/LABA group (49% versus 61%, respectively), but the number of smoking pack-years was similar in both treatment groups (Table 1). Similarly, there was a smaller proportion of high-risk (Global initiative for chronic Obstructive Lung Disease (GOLD) D) patients in the UMEC+ICS/LABA group than in the PBO+ICS/LABA group (Table 1). However, the proportion of patients with GOLD Stage II−IV COPD in each of the two treatment groups was similar (Table 1). The UMEC+ICS/LABA group experienced a smaller number of COPD exacerbations 12 months before screening than in the PBO+ICS/LABA group (28 and 43, respectively; Table 1).
Outcomes
Primary end point
Compared with PBO+ICS/LABA, UMEC+ICS/LABA resulted in statistically significant and clinically meaningful improvements in change from baseline in trough FEV1 at Day 85 (123 ml, 95% confidence interval (CI): 71, 174; P<0.001; Table 2; Figure 2).
Secondary end points
UMEC+ICS/LABA resulted in statistically significant and clinically meaningful improvements in change from baseline in 0−6 h post-dose WM FEV1 at Day 84 compared with PBO+ICS/LABA (148 ml, 95% CI: 99, 197; P<0.001; Table 2).
Other end points
Statistically significant improvements in trough FEV1 were also observed at all other visits for UMEC+ICS/LABA compared with PBO+ICS/LABA (130 (95% CI: 91, 169)−154 ml (95% CI: 111, 198); P<0.001 for all; Figure 2).
Improvements for 0–6 h post-dose WM FEV1 similar to those observed at Day 84 were also observed at Days 1 and 28 for UMEC+ICS/LABA compared with PBO+ICS/LABA (123 ml, 95% CI: 89, 157; and 178 ml, 95% CI: 128, 228, respectively; P<0.001 for both days).
Forty-six percent of patients treated with UMEC+ICS/LABA had an increase in trough FEV1 of ⩾100 ml above baseline at Day 85 compared with 16% of patients treated with PBO+ICS/LABA (odds ratio (OR): 4.8, 95% CI: 2.6, 9.1; P<0.001; Table 2). The proportion of patients achieving an increase in FEV1 ⩾12% and ⩾200 ml in the first 6 h post dose on Day 1 was 56% and 24% in the groups UMEC+ICS/LABA and PBO+ICS/LABA, respectively (OR: 4.2, 95% CI: 2.4, 7.4;P<0.001; Table 2).
Statistically significant and clinically meaningful improvements in the change from baseline in FEV1 were observed at 15 min post dose on Day 84 for UMEC+ICS/LABA compared with PBO+ICS/LABA (127 ml, 95% CI: 75, 179; P<0.001). These improvements were maintained at 6 h post dose on Day 84 (156 ml, 95% CI: 107, 206; P<0.001; Supplementary Figure S1). Similar improvements were seen in the change from baseline in FEV1 with UMEC+ICS/LABA compared with PBO+ICS/LABA at 15 min post dose and 6 h post dose on Day 1 (66 ml; 95% CI: 40, 92; and 144 ml; 95% CI: 104, 185; respectively; P<0.001 for both), and at 15 min post dose and 6 h post dose on Day 28 (152 ml, 95% CI: 101, 203; and 180 ml, 95% CI: 123, 238; respectively; P<0.001 for both).
Statistically significantly greater change from baseline in peak FEV1 was demonstrated for UMEC+ICS/LABA compared with PBO+ICS/LABA at Day 84 (152 ml, 95% CI: 99, 205; P<0.001; Table 2). Similar improvements in peak FEV1 with UMEC+ICS/LABA compared with PBO+ICS/LABA were observed at Day 1 (125 ml, 95% CI: 89, 160; P<0.001) and Day 28 (180 ml, 95% CI: 128, 232; P<0.001).
Statistically significantly greater change from baseline in trough forced vital capacity (FVC) was demonstrated with UMEC+ICS/LABA compared with PBO+ICS/LABA at Day 85 (177 ml, 95% CI: 88, 267; P<0.001; Table 2). Similar improvements in trough FVC in change from baseline with UMEC+ICS/LABA compared with PBO+ICS/LABA were observed at Days 2, 28, 56 and 84 (165 (95% CI: 73, 257)−242 ml (95% CI: 165, 319); P<0.001 for all). Differences in serial FVC were statistically significantly greater for UMEC+ICS/LABA compared with PBO+ICS/LABA at all time points at Day 1 (113 (95% CI: 56, 170)−210 ml (95% CI: 136, 283); P<0.001 for all), Day 28 (196 (95% CI: 105, 287)−263 ml (95% CI: 166, 360); P<0.001 for all) and Day 84 (187 (95% CI: 87, 288)−234 ml (95% CI: 138, 329); P<0.001 for all).
For rescue medication use, UMEC+ICS/LABA resulted in a statistically significant reduction in change from baseline in mean puffs per day over weeks 1–12 versus PBO+ICS/LABA (−0.38, 95% CI: −0.67, −0.10; P<0.05; Table 2). However, no statistically significant difference was observed for percentage of rescue-free days for UMEC+ICS/LABA versus PBO+ICS/LABA (GSK data on file). Transition Dyspnoea Index (TDI) score at Day 84 was not significantly different for UMEC+ICS/LABA versus PBO+ICS/LABA (0.40, 95% CI: −0.15, 0.95; P=0.152; Table 2; Figure 3a). However, the mean TDI for the UMEC+ICS/LABA group exceeded the 1.0-unit threshold (1.07, s.e.: 0.197), which is considered the minimal clinically important difference for this end point,12 whereas the mean TDI in the PBO+ICS/LABA group (0.67, s.e.: 0.195) did not.
Least-squares mean (95% CI) change from baseline in (a) TDI score, (b) CAT score and (c) SGRQ score (ITT population). *P-values for treatment differences; CAT, COPD Assessment Test; CI, confidence interval; ICS, inhaled corticosteroid; ITT, intent-to-treat; LS, least squares; LABA, long-acting β2-agonist; PBO, placebo; SGRQ, St George’s Respiratory Questionnaire; TDI, Transition Dyspnoea Index; UMEC, umeclidinium.
Health-related quality of life
Statistically significant improvements from baseline in COPD Assessment Test (CAT) score (where a negative number denotes an improvement) were observed at Day 84 for UMEC+ICS/LABA versus PBO+ICS/LABA (−1.31, 95% CI: −2.59, −0.04; P<0.05; Table 2; Figure 3b). UMEC+ICS/LABA resulted in statistically significantly greater odds of being a CAT responder at Day 84 (OR: 2.71, 95% CI: 1.52, 4.85; P<0.001; Table 2) compared with PBO+ICS/LABA. Change from baseline in SGRQ total score at Day 84 was not statistically significantly different for UMEC+ICS/LABA versus PBO+ICS/LABA (−2.26, 95% CI: −4.77, 0.25; P=0.077; Table 2; Figure 3c). UMEC+ICS/LABA did not result in a statistically significantly greater odds of being an SGRQ responder (OR: 0.96, 95% CI: 0.56, 1.67; P=0.892; Table 2).
Safety
The incidence of adverse events (AEs) was similar between the UMEC+ICS/LABA (38%) and PBO+ICS/LABA (42%) treatment groups (Table 3). The most common AEs were nasopharyngitis, 13 and 15%, and headache, 3 and 7%, in the UMEC+ICS/LABA and PBO+ICS/LABA groups, respectively. Pneumonia was reported for 3 (3%) patients and 2 (2%) patients in the UMEC+ICS/LABA and PBO+ICS/LABA groups, respectively. Tachycardia was reported for a total of 2 (2%) patients in the PBO+ICS/LABA treatment group and none in the UMEC+ICS/LABA group. No other individual AE of special interest was reported in >1 (<1%) patient in each treatment group.
The number of on-treatment non-fatal serious AEs was similar between the UMEC+ICS/LABA and PBO+ICS/LABA treatment groups (6 (5%) and 4 (3%), respectively; Table 3). The number of patients who experienced COPD exacerbations was balanced between the UMEC+ICS/LABA and PBO+ICS/LABA groups (17 (14%) and 16 (14%), respectively; Table 3). There was one (<1%) fatality in the PBO+ICS/LABA group; this was not drug-related. No fatalities were reported in the UMEC+ICS/LABA group.
Post hoc analysis of trough FEV1
In the post hoc subgroup analyses of trough FEV1 by ICS/LABA subgroup, UMEC+FP/SAL 500/50 mcg resulted in a statistically significant improvement in change from baseline in trough FEV1 at Day 85 versus PBO+FP/SAL 500/50 mcg (156 ml, 95% CI: 77, 235; P<0.001; n=42 in each treatment group). UMEC+BD/FOR also resulted in statistically significant improvement in change from baseline in trough FEV1 at Day 85 versus PBO+BD/FOR (130 ml, 95% CI: 55, 204; P<0.001; n=49 in each treatment group). No statistically significant difference was observed for change from baseline in trough FEV1 at Day 85 with UMEC added to other ICS/LABA combinations (50 ml, 95% CI: −106, 207; P=0.519; n=18 and n=19 in the UMEC+ICS/LABA and PBO+ICS/LABA groups, respectively).
Discussion
Main findings
As limited prospective data are available on the efficacy of UMEC added to ICS/LABA combinations, this study aimed to build on and expand the available data set on open-label triple therapy. This study demonstrated statistically significant and clinically meaningful improvements in trough FEV1 at Day 85 with UMEC+ICS/LABA compared with PBO+ICS/LABA in patients with moderate-to-very-severe COPD who remained symptomatic on a range of different ICS/LABAs. These ICS/LABA combinations included FP/SAL 500/50 mcg (GSK) and BD/FOR (AstraZeneca), as they are among the most widely used ICS/LABAs. Other ICS/LABA combinations, including generics, were also included. Significant improvements in 0–6 h post-dose WM FEV1 after 12 weeks of treatment were also observed.
All treatments in this study were well-tolerated, and the incidence of AEs was similar between the UMEC+ICS/LABA (38%) and PBO+ICS/LABA (42%) treatment groups. No additional safety concerns were identified with the addition of UMEC to ICS/LABA.
In a post hoc subgroup analysis of the primary end point of trough FEV1 at Day 85 by ICS/LABA type, statistically significant improvements in FEV1 were observed in the FP/SAL 500/50 mcg and BD/FOR subgroups but not in the smaller subgroup including other ICS/LABAs (including generics). The improvements observed in trough FEV1 with UMEC+FP/SAL 500/50 mcg and UMEC+BD/FOR were similar and were also consistent with those seen in previous studies of UMEC added to FP/SAL 250/50 mcg twice daily7 and UMEC added to FF/VI 100/25 mcg once daily.6 These findings suggest that the choice of background ICS/LABA therapy is unlikely to have any impact on the add-on efficacy of UMEC 62.5 mcg when used as triple therapy in patients who remain symptomatic on ICS/LABA therapy. The lack of a significant difference observed between UMEC+ ICS/LABA and the PBO+ICS/LABA for the other ICS/LABA subgroup may have been related to the small number of patients who received other ICS/LABA combinations in this study.
Interpretation of findings in relation to previously published work
This study was specifically designed to examine the effect of the addition of UMEC to ICS/LABA on lung function. In addition, the study assessed the treatment difference in subjective PROs including TDI focal score and CAT score for the first time. However, the study was not formally powered to detect treatment differences in PRO measures. Despite the potential underpowering of this study to assess PROs, a statistically significant improvement was observed in CAT score after 12 weeks, with 20% more patients experiencing a clinically relevant improvement (⩾2-unit change13) in CAT score. The mean improvement in the TDI focal score showed a clinically relevant improvement in breathlessness (>1-unit change12) from baseline in the UMEC+ICS/LABA group but not in the PBO+ICS/LABA group. However, a statistically significant treatment difference for TDI score was not observed. The mean improvement in the total SGRQ score with UMEC 62.5 mcg triple therapy compared with ICS/LABA alone was statistically significant at Week 4, but not at Week 12; however, the magnitude of the treatment effect was similar at both visits and was in line with the other larger UMEC+ICS/LABA studies previously reported.6 As seen in other studies of UMEC+ICS/LABA, statistically significant reductions in the number of puffs per day of rescue medication use, an indirect measure of daily symptoms, were seen with UMEC+ICS/LABA versus PBO+ICS/LABA.6–8 UMEC monotherapy has been shown to provide meaningful improvements in PROs such as SGRQ.14 The improvements observed in this study were not consistent across PRO measures and did not reach reported minimal clinically important differences, possibly because all baseline PROs were measured while patients were receiving ICS/LABA.
Strengths and limitations of this study
Strengths of the current study include the range of ICS/LABAs that patients were initially receiving, which has not been included in previous UMEC add-on studies.4,6 However, there are also limitations of this study that should be considered. The study was not powered to detect differences in end point results between treatment groups in the different ICS/LABA subgroups. Although the post hoc sensitivity analysis reached statistical significance for differences in trough FEV1 in UMEC+ICS/LABA versus PBO+ICS/LABA in two of the ICS/LABA types (FP/SAL 500/50 mcg and BD/FOR), which were relatively small samples, the number of patients in the other ICS/LABA subgroup was inconclusive because of very small sample sizes.
Finally, this study only assessed COPD exacerbations as a safety outcome over the relatively short 3-month follow-up period. The patients in this study may not have been at risk of exacerbation during the trial, as they did not require a history of exacerbation to enter the trial. Exacerbations were reported in a similar number of patients on both regimens as safety outcomes in the current analysis. A duration longer than 12 weeks, in a much larger population, would be recommended to assess the effect of UMEC added to ICS/LABA on COPD exacerbations as an efficacy end point. However, a large pooled integrated analysis of four previous UMEC 62.5 mcg+ICS/LABA 12-week trials, performed in patients with and without an exacerbation history, has demonstrated a benefit of UMEC triple therapy versus ICS/LABA alone in reducing the risk of a first moderate/severe COPD exacerbation.8,9
Implications for future research policy and practice
Several placebo-controlled randomised studies have addressed the efficacy of UMEC in improving lung function and symptoms when given as a monotherapy14,15 or add-on therapy to ICS/LABA.7,8 However, future studies comparing UMEC with other LAMAs as monotherapy or in addition to ICS/LABA are warranted.
As the current study was not powered to detect differences in PRO measurements, further studies are needed to investigate the effect of UMEC on these measures.
Long-term exacerbation studies are also needed to document the benefits of UMEC-containing triple therapy compared with ICS/LABA therapy alone. The InforMing the PAthway of COPD Treatment (IMPACT; NCT02164513) exacerbation study, which is currently ongoing to evaluate the benefit of UMEC triple therapy versus both UMEC/VI or FF/VI, may answer these questions in a higher exacerbation risk COPD population.
Conclusions
In summary, UMEC added to an existing choice of ICS/LABA improved lung function, rescue medication use and CAT score, one measure of HRQoL, when compared with PBO in symptomatic patients with COPD. No additional safety concerns were identified with UMEC in this add-on setting.
Materials and methods
Study design
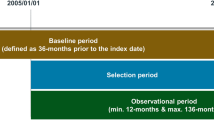
This was a 12-week, multicentre, randomised, double-blind, parallel-group study conducted between September 2014 and March 2015 in the Czech Republic, Germany, Greece and the Netherlands (GSK study number: 201314; ClinicalTrials.gov registration number: NCT02257372).
The study protocol and informed consent were reviewed and approved by a national, regional or investigational centre ethics committee or institutional review board, in accordance with Good Clinical Practice (GCP). This study was conducted in accordance with GCP and the ethical principles outlined in the Declaration of Helsinki.
Patients
Patients eligible for inclusion were ⩾40 years of age with an established clinical history of COPD, current or former smokers with ⩾10 pack-years smoking history, had a pre- and post-albuterol/salbutamol FEV1/FVC ratio of <0.7 and a pre- and post-albuterol/salbutamol FEV1 of ⩽70% of predicted normal values. Patients also had a dyspnoea score of ⩾2 on the modified Medical Research Council Dyspnoea Scale16 at Visit 1 and remained symptomatic after receiving one of the ICS/LABA combinations approved for COPD ⩾30 days before screening.
Exclusion criteria were a current diagnosis of asthma, hospitalisation for COPD or pneumonia within 12 weeks before Visit 1, lung volume reduction surgery within the 12 months before Visit 1, lower-respiratory-tract infection requiring antibiotic use within 6 weeks of Visit 1, use of long-term oxygen therapy (prescribed for >12 h per day) and participation in the acute phase of a pulmonary rehabilitation programme within 4 weeks before Visit 1. Additional exclusion criteria were evidence of concurrent respiratory disease or other clinically significant medical condition. This included an abnormal and clinically significant electrocardiogram finding at Visit 1 determined by atrial fibrillation with a rapid ventricular rate (>120 b.p.m.), ventricular tachycardia or second-degree heart block Mobitz type II or third-degree heart block (unless a pacemaker or defibrillator had been inserted). The use of prohibited medications (Supplementary Table S2) within the specified time periods also excluded patients from the study.
Study treatments
Patients must have been receiving ICS/LABA at doses and frequencies approved for COPD ⩾30 days before the run-in period of 7±2 days. The ICS/LABA combinations received in this study were as follows: FP/SAL 500/50 mcg twice daily, BD/FOR 200/6 mcg twice daily or 400/12 mcg twice daily, or any other ICS/LABA combinations including generics listed in Supplementary Table S1. It should be noted that patients receiving FP/SAL 250/50 mcg or FF/VI 100/25 mcg were not included in the current study, as previous studies have investigated these. After the run-in period, patients were randomised 1:1 to UMEC 62.5 mcg (delivering 55 mcg) once daily or PBO once daily, added to their open-label ICS/LABA twice daily for 12 weeks. UMEC and PBO were double-blinded and administered via the ELLIPTA inhaler (Duhram, NC, USA).
Randomisation was stratified by the type of open-label ICS/LABA administered (FP/SAL, BD/FOR or other ICS/LABA combinations including generics). Randomisation codes were generated by GSK using a validated computerised system (RandAll NG). Patients were randomised using an Interactive Voice Response System.
Outcomes
Primary end point
The primary efficacy end point was trough FEV1 on Day 85 (defined as the mean of the FEV1 values obtained 23 and 24 h after dosing on Day 84).
Secondary end points
The secondary end point was WM 0–6 h FEV1 at Day 84.
Other end points
Other efficacy end points included trough FEV1 and WM FEV1 over 0–6 h post dose at other time points, proportion of patients achieving an increase of ⩾100 ml above baseline in trough FEV1, proportion of patients achieving an increase in FEV1 of ⩾12% and ⩾200 ml above baseline at any time during 0–6 h post dose on Day 1, serial FEV1 over 0–6 h (at each time point); peak FEV1, and trough and serial FVC. Rescue albuterol/salbutamol use (mean puffs per day and percentage of rescue-free days) and TDI focal score at Day 84 were also measured.
HRQoL
Health-related quality of life (HRQoL) end points included CAT score,17,18 proportion of CAT responders (defined as a reduction from baseline of ⩾2 units in CAT score), St George’s Respiratory Questionnaire for COPD patients (SGRQ-C) score and the proportion of SGRQ responders (defined by a reduction from baseline of ⩾4 units in SGRQ score).19 SGRQ scores were calculated from the SGRQ-C scores using standardised adjustment.
Safety
Safety assessments included monitoring of AEs, clinical laboratory tests, vital signs, physical examinations and COPD exacerbations. A COPD exacerbation was defined as an acute worsening of symptoms of COPD requiring the use of any treatment beyond study medication or rescue albuterol/salbutamol.
Post hoc analysis
A post hoc sensitivity analysis of trough FEV1 at Day 85 was conducted by the ICS/LABA subgroup. Three subgroups were defined: FP/SAL 500/50 mcg, BD/FOR and other ICS/LABA combinations including generics.
Statistical analysis
Sample size calculations were based on the primary end point of trough FEV1 at Day 85. They assumed 90% power and a 2-sided 5% significance level with an estimate of residual standard deviation for trough FEV1 of 220 ml and a treatment difference of 100 ml. Under these assumptions, and to account for an estimated withdrawal rate of 10%, 115 evaluable patients on each treatment (230 in total) were required for 90% power to detect a 100 -ml difference between treatments in trough FEV1.
Three patient populations were identified: all patients enrolled population (all patients for whom a record existed on the study database), ITT population (all patients who were randomised to treatment and received at least one dose of randomised study medication) and per-protocol population (all patients in the ITT population who did not have a full protocol deviation considered to impact efficacy).
The UMEC+ICS/LABA versus PBO+ICS/LABA treatment comparison was performed on the primary end point. If statistical significance was demonstrated at the 5% level for the primary end point, then inferences on the secondary and other end points were made for the ITT population.
Primary end point trough FEV1 at Day 85 was analysed for the ITT population using a mixed model repeated measures analysis, including trough FEV1 recorded at each of Days 2, 28, 56, 84 and 85. The model included covariates of baseline FEV1, type of ICS/LABA (FP/SAL, BD/FOR or other), smoking status, day, treatment and day-by-baseline interaction, where day is nominal. A day-by-treatment interaction term was also included to allow treatment effects to be estimated at each visit separately.
The post hoc analyses of trough FEV1 at Day 85 by ICS/LABA subgroup were performed using a mixed model repeated measures analysis with covariates of treatment, baseline FEV1, smoking status, day, day-by-baseline and day-by-treatment interactions.
References
GOLD. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. Available at http://www.goldcopd.org (accessed on 12 August 2015) (2015).
World Health Organization. Burden of COPD. Available at http://www.who.int/respiratory/copd/burden/en/ (accessed on 19 August 2015) (2015).
James, G. D., Donaldson, G. C., Wedzicha, J. A. & Nazareth, I. Trends in management and outcomes of COPD patients in primary care, 2000-2009: a retrospective cohort study. NPJ. Prim. Care. Respir. Med. 24, 14015 (2014).
GSK. INCRUSE® ELLIPTA:TM highlights of prescribing information. Available at https://www.gsksource.com/pharma/content/dam/GlaxoSmithKline/US/en/Prescribing_Information/Incruse_Ellipta/pdf/INCRUSE-ELLIPTA-PI-PIL.PDF (accessed on 12 August 2015) (2014).
EMC. Summary of Product Characterstics: Incruse 55 micrograms inhalation powder. Available at https://www.medicines.org.uk/emc/medicine/29394 (accessed on 12 August 2015) (2015).
Siler, T. M. et al. Efficacy and safety of umeclidinium added to fluticasone furoate/vilanterol in chronic obstructive pulmonary disease: Results of two randomized studies. Respir. Med. 109, 1155–1163 (2015).
Siler, T. M., Kerwin, E., Singletary, K., Brooks, J. & Church, A. Efficacy and safety of umeclidinium added to fluticasone propionate/salmeterol in patients with COPD: results of two randomized, double-blind studies. COPD 9, 1–10 (2015).
Siler, T. et al. Triple therapy with umeclidinium plus fixed-combination inhaled corticosteroid/long-acting β2-agonist therapy in chronic obstructive pulmonary disease: pooled results in placebo-controlled trials. Am. J. Respir. Crit. Care Med. 191, A5778 (2015).
Kerwin, E. et al. Triple therapy of umeclidinium and inhaled corticosteroid/long-acting β2-agonist (ICS/LABA) versus placebo+ICS/LABA in GOLD D patients. Eur. Respir. J. 46(Suppl 1): PA1490 (2015).
Kew, K. M. & Seniukovich, A. Inhaled steroids and risk of pneumonia for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 3, CD010115 (2014).
EMC. Summary of Product Characterstics: Seretide 100, 250, 500 Accuhaler. Available at https://www.medicines.org.uk/emc/medicine/2317/SPC/Seretide+100,+250,+500+Accuhaler (accessed on 23 March 2016) (2015).
Witek, T. J. Jr & Mahler, D. A. Minimal important difference of the transition dyspnoea index in a multinational clinical trial. Eur. Respir. J. 21, 267–272 (2003).
Kon, S. S. et al. Minimum clinically important difference for the COPD Assessment Test: a prospective analysis. Lancet Respir. Med. 2, 195–203 (2014).
Trivedi, R., Richard, N., Mehta, R. & Church, A. Umeclidinium in patients with COPD: a randomised, placebo-controlled study. Eur. Respir. J. 43, 72–81 (2014).
Donohue, J. F. et al. Efficacy and safety of once-daily umeclidinium/vilanterol 62.5/25 mcg in COPD. Respir. Med. 107, 1538–1546 (2013).
UNC. Modified medical research council dyspnea scale. Available at http://www.cscc.unc.edu/spir/public/UNLICOMMMRCModifiedMedicalResearchCouncilDyspneaScale08252011.pdf (accessed on 2 December 2015) (2012).
Jones, P. W. et al. Tests of the responsiveness of the COPD assessment test following acute exacerbation and pulmonary rehabilitation. Chest 142, 134–140 (2012).
Jones, P. W. et al. Development and first validation of the COPD Assessment Test. Eur. Respir. J. 34, 648–654 (2009).
Jones, P. W. St George's respiratory questionnaire: MCID. COPD 2, 75–79 (2005).
Acknowledgements
This study was funded and conducted by GSK (GSK study number: 201314). Medical writing assistance was provided by Joanne Ashworth and Matthew Robinson of Fishawack Indicia, funded by GSK. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole and have given final approval to the version to be published.
Funding
This study was funded by GSK (GSK study number: 201314; ClinicalTrials.gov NCT02257372).
Author information
Authors and Affiliations
Contributions
A.R.S., J.H.R., A.C. and C.Q.Z. designed the study and undertook the data analysis and interpretation. W.A.F. and Y.S.P. undertook the data analysis and interpretation. All authors contributed in the drafting of the paper. A.R.S. was the study accountable person.
Corresponding author
Ethics declarations
Competing interests
A.R.S., J.H.R., A.C., C.Q.Z., Y.S.P. and W.A.F. are employees of GSK and hold stocks/shares in GSK. GSK (the study sponsor) was involved with the design of the study, collection and analysis of data and decision to publish.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Sousa, A., Riley, J., Church, A. et al. The effect of umeclidinium added to inhaled corticosteroid/long-acting β2-agonist in patients with symptomatic COPD: a randomised, double-blind, parallel-group study. npj Prim Care Resp Med 26, 16031 (2016). https://doi.org/10.1038/npjpcrm.2016.31
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/npjpcrm.2016.31
This article is cited by
-
Eligibility of patients with chronic obstructive pulmonary disease for inclusion in randomised control trials investigating triple therapy: a study using routinely collected data
Respiratory Research (2024)
-
Letter to the Editor Regarding “Fluticasone Furoate/Umeclidinium/Vilanterol (FF/UMEC/VI) Triple Therapy Compared with Other Therapies for the Treatment of COPD: A Network Meta-Analysis”
Advances in Therapy (2023)